THE EXCHANGE | Newsletter February 2019
Robots Chip in to Aid Kidney Transplant
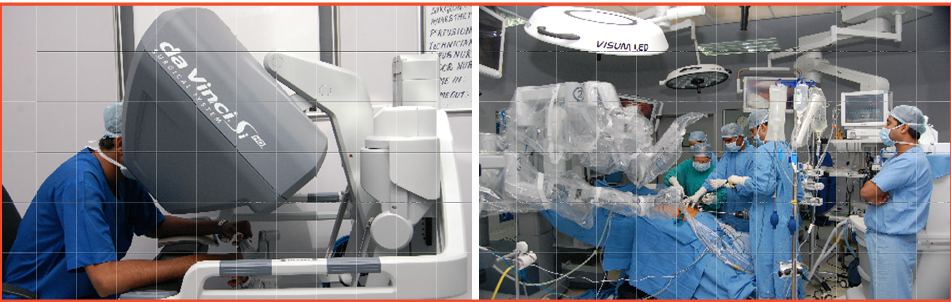
The Medanta Kidney and Urology Institute was initiated by experienced teams of Urologist and Nephrologists led by medical stalwarts, Dr. Rajesh Ahlawat and Dr. Vijay Kher. Since early days, the Institute was equipped with latest, state-of-the-art technology such as the Da Vinci robot to deliver precise, customized patient care.
The team at Medanta has performed over 2500 robotic surgeries and 2000 kidney transplants. Since the year 2000, all donor nephrectomies have been performed laparoscopically. To extend the benefits of minimally invasive surgery to kidney transplant patients, surgical expertise of kidney transplant was combined with robotic surgery using the Da Vinci robot.
Robotic Kidney Transplantation was conceptualized in 2012 as a collaborative effort between teams of Vattikuti Urology Institute, Henry Ford Hospital, Detroit (USA), and Medanta Kidney and Urology Institute, Gurugram. Within the framework of IDEAL guidelines, phase 0 (preclinical studies on cadavers), phase 1 and phase 2 trials were successfully conducted proving the feasibility and safety of the procedure.
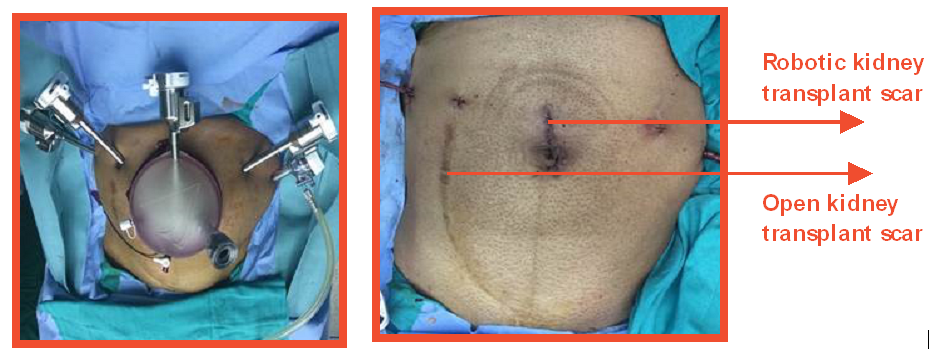
The process was gradually improvised to optimize patient benefit. An important innovation was the introduction of the hypothermia technique using ice slush to keep the kidneys cool while they were being transplanted robotically. The improvement in renal function using the ice slush regional hypothermia was similar to open kidney transplants. Another technique was innovated to fix the grafts in position so that they would be accessible for percutaneous biopsies during the post-transplant period. The results were published in various international peer reviewed journals.
Over the years, Dr. Ahlawat has demonstrated and initiated the robotic kidney transplant program at several international and Indian platforms. The technique has gained wide acceptance with encouraging results benefitting hundreds of kidney transplant patients. This has also resulted in fewer procedure related complications.
In a robotic procedure, the technology, powered by robotics, translates the surgeon's hand movements into smaller, precise movements of miniscule instruments inside a patient's body. The advanced camera provides 3D vision and higher magnification that enhances the visibility of the surgical area, improving accuracy and precision of the surgeon who stays in control of the system at all times.
The team at Medanta has performed almost 300 robotic kidney transplants with great outcomes. At one-year follow-up, patient survival is 95%, whereas the graft survival is 93.6%. Death censored graft survival has been reported as 98.6%. The procedure has been safely performed with reduced complications, blood loss and pain, leading to early recovery and discharge, while having graft function comparable to open kidney transplant.
Case Study
A 36-year-old man who had undergone open kidney transplant in 2004 with his mother as a donor had been struggling for one year because of graft failure. He had been on dialysis for a year and was in immediate need of a second transplant. Apprehensive of the painful and long post-operative recovery that followed his earlier transplant, he was looking for a better alternative. Meeting the transplant team led by Dr. Rajesh Ahlawat and Dr. Vijay Kher, and other patients who had undergone robotic kidney transplant at Medanta inspired the confidence of undergoing a second transplant robotically. With his father as the donor, the patient underwent robotic kidney transplant in 2016.
His post-operative recovery was uneventful. The patient was ambulatory the same day. He experienced much lesser pain as compared to the earlier open transplant procedure. He did not require higher dose of analgesics. His graft kidney recovered very well and he was discharged in six days with a creatinine of 1.2.
Learn more https://bit.ly/2B6v8au
https://www.medanta.org/dr-rajesh-ahlawat/
https://www.medanta.org/dr-vijay-kher/
https://www.medanta.org/dr-feroz-amir-zafar/
Pregnancy Safe in Breast Cancer Survivors
Breast cancer is the most common cancer reported by women of reproductive age. The leading cancer of urban India has surpassed the incidence of cervical cancer. A survey conducted in metro cities in India by the Indian Council of Medical Research (ICMR) indicated that the incidence of breast cancer almost doubled between the period 1982 and 2005, and that the disease affects Indian women a decade before it mostly strikes their western counterparts.
Changing lifestyle pattern of urban women is increasingly resulting in delayed childbirth. In several cases, breast cancer affects young women even before the reproductive process. Young breast cancer survivors may experience infertility due to chemotherapy-related gonadotoxicity. Also, delay in childbearing is mandatory when these women are on the recommended five years of hormonal therapy post-recovery. This has a significant impact on the quality of life causing substantial distress in affected, young women. Owing to the disease associated stigma, parents of young girls diagnosed with breast cancer are often worried more about marriage and fertility issues than the disease and its treatment.
While almost 50% of young women newly diagnosed with breast cancer report interest in having children, less than 10% are able to conceive after finishing treatment. In fact, of all cancer survivors, breast cancer survivors are the least likely to have a baby after diagnosis.
Case Study
28-year-old Paula was diagnosed with breast cancer in 2013. She had a strong family history of breast cancer and was also found to be positive for the BRCA 2 gene that increases the risk of breast and ovarian cancer. Keen to preserve her fertility, she opted to freeze her eggs before she started on chemotherapy. Patients who have an identified gene mutation are recommended to undergo risk reducing surgeries such as removal of breasts and ovaries. Keen on having a baby and nursing her, she insisted on delaying both the risk reducing surgeries until she completed her family. Post-treatment, Paula was on hormone blocking therapy for four years, following which she conceived naturally and delivered a healthy baby.
https://www.medanta.org/dr-kanchan-kaur/
Contoura Vision - The Next Revolution in LASIK
Contoura Vision Topography Guided LASIK corrects the vision based on the eye's unique attributes as against the standard LASIK surgery in which the vision correction is based only on spectacle or contact lens prescription. The technology has unparalleled diagnostic capabilities to record even the minutest imperfections in the curvature of the cornea. It provides measurement of 22,000 points as compared to the currently available wave front-guided LASIK that measures around 200 points. Hence this is a an unprecedented technology as it corrects the refractive errors with highest precision.
Contoura Vision Topography Guided LASIK involves the use of a separate diagnostic device called Topolyzer apart from the conventional refractive Suite. The corneal topography images captured by this device are transferred through the wavenet to the treatment planning station. These topography maps guide in creating customised treatment profile for each patient which is then executed using the state-of-the-art excimer laser.
Food and Drug Administration (FDA) results reveal that the patients who opted for this technology recorded a significant improvement and were able to see even more clearly without corrective eyewear. As per the clinical trials statistics, almost 90% of patients post-operatively saw as well or better without glasses than they ever did with glasses.
Benefits:
- Reduced difficulty during night driving
- Reduced sensitivity towards light
- Less glare
- Better quality vision
https://www.medanta.org/dr-sudipto-pakrasi/
Robots Chip in to Aid Kidney Transplant
The Medanta Kidney and Urology Institute was initiated by experienced teams of Urologist and Nephrologists led by medical stalwarts, Dr. Rajesh Ahlawat and Dr. Vijay Kher. Since early days, the Institute was equipped with latest, state-of-the-art technology such as the Da Vinci robot to deliver precise, customized patient care.
The team at Medanta has performed over 2500 robotic surgeries and 2000 kidney transplants. Since the year 2000, all donor nephrectomies have been performed laparoscopically. To extend the benefits of minimally invasive surgery to kidney transplant patients, surgical expertise of kidney transplant was combined with robotic surgery using the Da Vinci robot.
Robotic Kidney Transplantation was conceptualized in 2012 as a collaborative effort between teams of Vattikuti Urology Institute, Henry Ford Hospital, Detroit (USA), and Medanta Kidney and Urology Institute, Gurugram. Within the framework of IDEAL guidelines, phase 0 (preclinical studies on cadavers), phase 1 and phase 2 trials were successfully conducted proving the feasibility and safety of the procedure.
The process was gradually improvised to optimize patient benefit. An important innovation was the introduction of the hypothermia technique using ice slush to keep the kidneys cool while they were being transplanted robotically. The improvement in renal function using the ice slush regional hypothermia was similar to open kidney transplants. Another technique was innovated to fix the grafts in position so that they would be accessible for percutaneous biopsies during the post-transplant period. The results were published in various international peer reviewed journals.
Over the years, Dr. Ahlawat has demonstrated and initiated the robotic kidney transplant program at several international and Indian platforms. The technique has gained wide acceptance with encouraging results benefitting hundreds of kidney transplant patients. This has also resulted in fewer procedure related complications.
In a robotic procedure, the technology, powered by robotics, translates the surgeon's hand movements into smaller, precise movements of miniscule instruments inside a patient's body. The advanced camera provides 3D vision and higher magnification that enhances the visibility of the surgical area, improving accuracy and precision of the surgeon who stays in control of the system at all times.
The team at Medanta has performed almost 300 robotic kidney transplants with great outcomes. At one-year follow-up, patient survival is 95%, whereas the graft survival is 93.6%. Death censored graft survival has been reported as 98.6%. The procedure has been safely performed with reduced complications, blood loss and pain, leading to early recovery and discharge, while having graft function comparable to open kidney transplant.
Case Study
A 36-year-old man who had undergone open kidney transplant in 2004 with his mother as a donor had been struggling for one year because of graft failure. He had been on dialysis for a year and was in immediate need of a second transplant. Apprehensive of the painful and long post-operative recovery that followed his earlier transplant, he was looking for a better alternative. Meeting the transplant team led by Dr. Rajesh Ahlawat and Dr. Vijay Kher, and other patients who had undergone robotic kidney transplant at Medanta inspired the confidence of undergoing a second transplant robotically. With his father as the donor, the patient underwent robotic kidney transplant in 2016.
His post-operative recovery was uneventful. The patient was ambulatory the same day. He experienced much lesser pain as compared to the earlier open transplant procedure. He did not require higher dose of analgesics. His graft kidney recovered very well and he was discharged in six days with a creatinine of 1.2.
Learn more https://bit.ly/2B6v8au
https://www.medanta.org/dr-rajesh-ahlawat/
https://www.medanta.org/dr-vijay-kher/
https://www.medanta.org/dr-feroz-amir-zafar/
Pregnancy Safe in Breast Cancer Survivors
Breast cancer is the most common cancer reported by women of reproductive age. The leading cancer of urban India has surpassed the incidence of cervical cancer. A survey conducted in metro cities in India by the Indian Council of Medical Research (ICMR) indicated that the incidence of breast cancer almost doubled between the period 1982 and 2005, and that the disease affects Indian women a decade before it mostly strikes their western counterparts.
Changing lifestyle pattern of urban women is increasingly resulting in delayed childbirth. In several cases, breast cancer affects young women even before the reproductive process. Young breast cancer survivors may experience infertility due to chemotherapy-related gonadotoxicity. Also, delay in childbearing is mandatory when these women are on the recommended five years of hormonal therapy post-recovery. This has a significant impact on the quality of life causing substantial distress in affected, young women. Owing to the disease associated stigma, parents of young girls diagnosed with breast cancer are often worried more about marriage and fertility issues than the disease and its treatment.
While almost 50% of young women newly diagnosed with breast cancer report interest in having children, less than 10% are able to conceive after finishing treatment. In fact, of all cancer survivors, breast cancer survivors are the least likely to have a baby after diagnosis.
Case Study
28-year-old Paula was diagnosed with breast cancer in 2013. She had a strong family history of breast cancer and was also found to be positive for the BRCA 2 gene that increases the risk of breast and ovarian cancer. Keen to preserve her fertility, she opted to freeze her eggs before she started on chemotherapy. Patients who have an identified gene mutation are recommended to undergo risk reducing surgeries such as removal of breasts and ovaries. Keen on having a baby and nursing her, she insisted on delaying both the risk reducing surgeries until she completed her family. Post-treatment, Paula was on hormone blocking therapy for four years, following which she conceived naturally and delivered a healthy baby.

https://www.medanta.org/dr-kanchan-kaur/
Contoura Vision - The Next Revolution in LASIK
Contoura Vision Topography Guided LASIK corrects the vision based on the eye's unique attributes as against the standard LASIK surgery in which the vision correction is based only on spectacle or contact lens prescription. The technology has unparalleled diagnostic capabilities to record even the minutest imperfections in the curvature of the cornea. It provides measurement of 22,000 points as compared to the currently available wave front-guided LASIK that measures around 200 points. Hence this is a an unprecedented technology as it corrects the refractive errors with highest precision.
Contoura Vision Topography Guided LASIK involves the use of a separate diagnostic device called Topolyzer apart from the conventional refractive Suite. The corneal topography images captured by this device are transferred through the wavenet to the treatment planning station. These topography maps guide in creating customised treatment profile for each patient which is then executed using the state-of-the-art excimer laser.
Food and Drug Administration (FDA) results reveal that the patients who opted for this technology recorded a significant improvement and were able to see even more clearly without corrective eyewear. As per the clinical trials statistics, almost 90% of patients post-operatively saw as well or better without glasses than they ever did with glasses.
Benefits:
- Reduced difficulty during night driving
- Reduced sensitivity towards light
- Less glare
- Better quality vision






