THE EXCHANGE | Newsletter - Jan 2024
Medanta Gurugram First in India to Use Advanced AI-enabled Penumbra Lightning Technology for Treating Pulmonary Embolism
Venous thromboembolism (VTE) represents a significant and serious health burden worldwide. Percutaneous endovascular interventions have become a standard minimally invasive treatment for removal of blood clots. The Penumbra Lightning 12F catheter is an innovative AI-driven device specifically engineered to selectively enhance clot aspiration during percutaneous endovascular procedure.
We describe the successful utilisation of this new technology in a patient with life threatening lung clots, aka Pulmonary Embolism (PE), and leg clots, aka Deep Vein Thrombosis (DVT), to highlight the effectiveness and safety of the Penumbra Lightning 12F catheter.
Case Study
A 62-year-old male patient with chief complaints of acute leg pain and swelling with shortness of breath was flown in from Bhopal in a critical condition. He had a history of hypertension and smoking. Ultrasound colour Doppler imaging confirmed blood clots in the leg vein; a clot in the left lower lung was identified using a computed tomography (CT) angiography.
Due to the acute onset and extensive nature of the clotting event, the patient was considered for clot removal technique to achieve rapid and efficient clot removal with minimal blood loss. The Penumbra Lightning 12F catheter was chosen for its ability to navigate the tortuous venous anatomy and effectively aspirate the thrombus.
Under local anaesthesia, a small incision was made to access the left leg (femoral) vein. Through this access site, a 6F catheter was placed, and the Penumbra Lightning 12F catheter was advanced over a guide wire to the site of the clot.

The catheter's aspiration system was activated and intermittent clot aspiration was performed. The procedure was guided by X-ray and intravascular ultrasound (IVUS) to ensure precise catheter positioning and thrombus removal.
The Penumbra Lightning catheter facilitated efficient thrombus aspiration, resulting in a significant reduction in clot burden in the left iliac and leg (femoral) veins. Follow-up ultrasound colour Doppler, performed immediately after the procedure, revealed substantial reduction in the clot size.
The patient reported immediate relief from shortness of breath, leg pain and swelling. The post-procedural course was uneventful, and the patient was discharged on Day 2 after the procedure on blood thinning tablets (anticoagulation therapy) with instructions for outpatient follow-up.
The patient has recovered well and has reported significant improvement in his quality of life.
Conclusion
Through this case, we could see the Penumbra Lightning 12F catheter’s efficacy in percutaneous endovascular management of blood clots in the legs and lungs, with immediate alleviation of symptoms. Its large-bore design, combined with excellent navigability, allows effective clot aspiration, reducing the need for additional interventions. The minimally invasive nature of this endovascular procedure helps shorten hospital stays and hastens recovery. The catheter's design and functionality make it a valuable tool for vascular specialists dealing with complex thromboembolic cases.
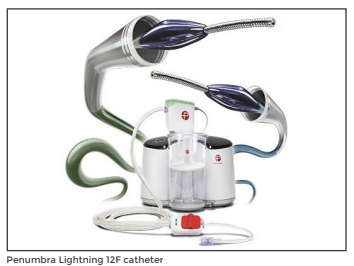
Advanced AI-enabled Penumbra Lightning 12F Catheter
“Medanta - Gurugram has introduced the Penumbra Lightning 12F Catheter - an AI-driven device revolutionising selective clot removal in endovascular procedures. As the first hospital in India to adopt this technology, Medanta has successfully treated 25 cases of pulmonary embolism since July 2023. Powered by AI, this technology minimises blood loss, reducing complications, such as anaemia, in addition to expediting patient recovery.
The introduction of this technology signifies a remarkable advancement in aiding individuals afflicted by pulmonary embolism, enabling faster recovery and improved outcomes. In our endeavour to improve awareness surrounding this critical condition, Medanta has piloted the Pulmonary Embolism Interventions and Response Team (PEiRT-Bharat) programme. This programme is dedicated to raising awareness about reducing the incidence of pulmonary embolism in India, the available treatment options, and enhancing health outcomes. The PEiRT-Bharat programme is helmed by a specialised team comprising critical care experts, vascular and cardiac surgeons, cardiologists, haematologists, respiratory physicians, and general practitioners.”
Dr. Naresh Trehan
Chairman and Managing Director
Medanta
Dr. Tarun Grover
Director - Peripheral Vascular and Endovascular Sciences
Medanta - Gurugram
Dr. Rajiv Parakh
Chairman - Peripheral Vascular and Endovascular Sciences
Medanta - Gurugram
Medanta @ Work
A Case of Acute Myeloid Leukaemia Presenting During Pregnancy
Incidence of acute myeloid leukaemia (AML) in pregnancy is about 1 in 75,000 to 1,00,000 accounting for two-third of all leukaemia cases reported in pregnancy. The median age of diagnosis is 32 years; median survival without treatment is 6 months. With treatment, 5-year survival rate is 26%, and 50%-80% adults achieve remission. AML during pregnancy presents dilemmas and challenges. There are no clear guidelines and the data is sparse. Chemotherapy poses risks to the developing foetus while delaying chemotherapy worsens prognosis. We present a case of AML that was diagnosed at 22 weeks and 6 days of the pregnancy.
Case Study
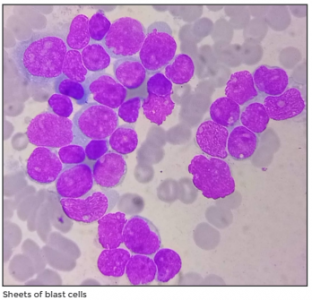
A 33-year-old female, 22-weeks-and-6-days pregnant, presented to Medanta - Gurugram with high-grade fever for 3 days. She had a history of one spontaneous miscarriage 4 years back, an uncomplicated pregnancy with vaginal delivery 1.5 years back, and no other significant past history. Her systemic examination was normal with a 22-week uterus and a normal foetal heartbeat. The patient had an uncomplicated pregnancy with unremarkable investigations till 3 days back when she developed fever. Laboratory tests revealed haemoglobin (Hb) of 7.9 g/dl, total leukocyte count (TLC) of 40140 with 90% blast cells and 68,000 platelets. Subsequently, immunoflow cytometry test confirmed the diagnosis of AML with the genetic mutation aberrant CD7 karyotype.
A multidisciplinary team (MDT) was formed involving haemato-oncologist, obstetrician, neonatologist and foetal medicine specialist to decide the best course of action.
In view of possible bad prognosis if chemotherapy was delayed, induction chemotherapy with Danorubicin and Cytarabine (7+3) was started after counselling the couple regarding the risks of chemotherapy on foetus and risk of maternal sepsis.

Foetus was monitored with daily heartbeat recording and weekly ultrasounds. The patient received blood transfusions as her Hb and platelet counts were low due to chemotherapy. In addition, she was also given preventive antibiotics and supportive medicines. Later, she developed high fever, breathlessness and cough due to fungal pneumonia, for which antifungals were administered. Post chemotherapy, bone marrow biopsy showed 39% blast cells with paucity of normal haematopoietic cells indicating non-remission.
In view of non-remission, additional supportive chemotherapy was indicated, which poses additional risk to the foetus such as sepsis and sudden death.
An MDT meeting was held, and, with the couple’s consent, it was decided to deliver the baby by a caesarean section before starting additional chemotherapy considering that the pregnancy was beyond the age of viability at that time. Before the procedure, steroid injections were given for lung maturity and MgSO4 drip for neuro protection. A 1.4 kg baby was delivered by lower segment caesarean section at 29 weeks and 4 days of gestation.
In her postoperative period, the patient received antibiotics and blood products due to low counts. Other than this, her postoperative period was uneventful and she recovered well. Supportive chemotherapy with Azacitadine and Venetoclux was started on Day 7 after the surgery.
Post delivery, the infant was admitted to the Neonatal Intensive Care Unit (NICU) as he required continuous positive airway pressure (CPAP), blood products, and intervention for intermittent apnoea. The infant recovered well and was discharged from the NICU after 54 days.
Discussion
AML during pregnancy poses dilemmas such as timing the chemotherapy and delivery. Chemotherapy can cause foeto-maternal sepsis, Sheets of blast cellsfoetal loss, growth restriction and prolonged NICU stay for the infant. However, delaying chemotherapy worsens the prognosis for the mother. AML in itself can cause growth restriction due to placental thrombosis, hyperleukocytosis and disseminated intravascular coagulation (DIC).
It is prudent to plan the delivery in between courses of chemotherapy after maternal bone marrow reconstitution as this avoids maternal and foetal sepsis and pancytopenia.
When chemotherapy is administered for AML during pregnancy, foetal loss occurs in 40% pregnancies in first trimester, and 10% in second trimester. Ninety percent foetus survive when chemotherapy is given after 28 weeks pregnancy. In our patient, AML was diagnosed in the second trimester and remission wasn’t achieved with first cycle of chemotherapy. Hence, delivery had to be planned after completing 28 weeks, just before administering additional chemotherapy.
At 28 weeks, the risk due to prematurity, developmental delay and prolonged NICU remain. So, careful timing of delivery is important to achieve the best possible outcome. In our case, the baby is doing well and the patient is now being planned for bone marrow transplantation.
Dr. Pooja Mittal
Senior Consultant - Obstetrics and Gynaecology, Institute of Women and Children
Medanta - Gurugram
Dr. T. J. Antony
Director and HOD - Neonatology and NICU, Paediatrics, Institute of Women and Children
Medanta - Gurugram
Dr. Nitin Sood
Director - Haemato Oncology and Bone Marrow Transplant, Cancer Institute
Medanta - Gurugram
Techbyte
Whole Exome Sequencing: A New Device in Clinical Investigative Toolbox
Many clinical disorders and diseases have an underlying genetic basis wherein a mutation in a specific gene coding for a particular protein results in alteration in the protein structure and function that in turn is responsible for the clinical disorder.
Whole Exome Sequencing (WES) is a technique for sequencing all the protein-coding regions (exons) of genes in a genome to identify the genetic variation responsible for the disease. It has emerged as a reasonably priced tool that helps not only in the diagnosis in an index patient but also helps in prognosticating the disease, guiding treatment, and identification of those at risk in asymptomatic family members of the patient.
We report a patient who presented to us recently and WES helped in establishing the genetic diagnosis for cardiac channelopathy and guiding appropriate treatment.
Case Study
A 5-year-old girl presented to Medanta - Gurugram a year after getting a cardiac arrest from which she was successfully resuscitated in her native country. At the time of cardiac arrest, she was on multiple medications, including antibiotics prescribed for COVID-19. Her electrocardiogram (ECG), done after resuscitation, revealed markedly prolonged QT interval. She was also found to have severe left ventricular dysfunction on echocardiography (Echo) that normalised within three weeks. She recovered with mild right hemiparesis and the magnetic resonance imaging (MRI) of her brain showed findings suggestive of hypoxic-ischemic encephalopathy.
There was no family history of similar illness or sudden cardiac death in first-degree relatives, including her only sibling – an elder brother. Even the ECGs of her parents and brother were normal. Based on the clinical diagnosis of congenital long QT syndrome (LQTS), she was started on Propranolol, but had two episodes of syncope in the following year, from which she recovered spontaneously. She was referred to us for
implantable cardioverter defibrillator (ICD) device.
On presentation to Medanta - Gurugram, she was stable with normal vital signs and neurological examination. Her ECG and Echo were normal. A diagnosis of congenital long QT syndrome was made and the dose of Propranolol was up-titrated. A 24-hour Holter test did not reveal any significant arrhythmias and the routine lab biochemistry tests of calcium, magnesium and potassium levels were normal.
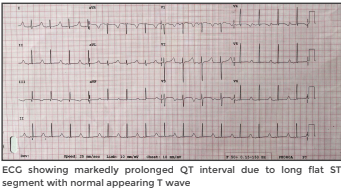
Hence, we did Whole Exome Sequencing for her, and the result revealed a pathogenic variant -SCN5A gene mutation, specifically a missense mutation 3-38647549-C-T that causes amino acid change on Val411Met on the SCN5A protein resulting in disruption of flow of sodium ions into the cardiac muscle. This mutation is autosomal dominant in inheritance and is seen in ion channel defects most common of which are the Brugada Syndrome and Congenital LQTS Type 3.
Based on the clinical and genetic diagnosis of LQTS-3, she was started on tablet Mexiletine that has been found to be useful in this subtype of LQTS. The QT interval decreased from a baseline of 580ms to 520ms – normal being up to 450ms – after a week. The patient was adviced to procure automatic external defibrillator and sent back to her country. ICD implantation was not performed at that time due to the inherent complexity and challenges of its use in small children and good clinical response with Propranolol and Mexiletine. Her parents’ blood samples were also taken for genetically studying the specific mutation.
Discussion
SCN5A gene mutation can result in LQTS-3 and Brugada Syndrome, both of which are ion channelopathies that can result in syncope and sudden cardiac death, but can be easily differentiated from each other by the ECG patterns. The ECG in Brugada Syndrome is characterised by coved ST segment elevations in leads V1 to V3 with T wave inversion, whereas in LQTS-3 there is markedly prolonged QT interval due to delayed onset of T wave and long flat ST segment.
LQTS has been classified with at least 16 subtypes based on the genetic mutation, although most clinical cases of LQTS are of types 1, 2 and 3. Some ECG features may help in distinguishing the type of LQTS, however, there is a large overlap. LQTS-3 patients have the longest QT interval amongst the three common subtypes, and present with episodes of syncope or cardiac arrest during sleep. The episodes are due to the occurrence of polymorphic ventricular tachycardia, and are more lethal than in other LQTS subtypes. Although, beta-blockers are useful in most subtypes of LQTS, Mexiletine has been found to particularly reduce the QT interval in LQTS-3.
The management of LQTS involves drug therapy (betablockers – propranolol, nadolol, mexiletine), surgical sympathectomy, and pacemaker or ICD implantation. The treatment strategy is personalised based on many factors, including the age, clinical presentation, family history of sudden death, genetic mutation, response to the medical therapy etc.
In the present case, genetic study in the form of WES not only helped in confirming the diagnosis, and establishing the subtype, but also in indicating a worse prognosis and guiding medical therapy.
Dr. Renu Saxena
Director and Head - Department of Pathology and Lab Medicine
Medanta - Gurugram
Dr. Shalini Goel
Principal Consultant - Department of Pathology and Lab Medicine
Medanta - Gurugram
Dr. Kartikeya Bhargava
Senior Director - Electrophysiology and Pacing, Heart Institute
Medanta - Gurugram
Medanta's Mission TB-Free India
New Technology, New Partners
With a vision to advance Tuberculosis (TB) elimination, Medanta - Gurugram recently held the ‘NTEP Medanta North India TB Conference’ focusing on fostering new partnerships and adopting innovative technology like ultraportable X-Ray machines, artificial intelligence for TB radiology, and sophisticated molecular diagnostics that are set to revolutionise on-the-spot screening and diagnosis.

Dr. Naresh Trehan (Chairman and Managing Director, Medanta) welcomed the gathering
which included Dr. Dhruv Chaudhary (Chairman – Haryana Task Force for TB), and Dr. Virendra Yadav (Chief Medical Officer, Gurugram), in addition to Dr. Randeep Guleria (Chairman - Institute of Internal Medicine, and Respiratory & Sleep Medicine; Director - Medical Education, Medanta, Gurugram) and other specialists from Medanta’s Respiratory & Sleep Medicine department. The event showcased compact technologies being used as part of Mission TB-Free India – led by Dr. Bornali Dutta (Director – Pulmonary Medicine, Respiratory and Sleep Medicine, Medanta, Gurugram) – in underserved rural and urban areas of Haryana, Delhi and Uttar Pradesh. This was followed by engaging session by delegates from our partner firms.
Kudos

Medanta Lucknow's Department of Neurology earns the WSO Angels Award (Diamond Status) for top-notch stroke care. This recognition by the World Stroke Organization (WSO) is awarded to hospitals that not only meet criteria for treatment that optimises survival and recovery, but also establish systems driving continuous improvement.
Medanta - Lucknow is proud to have earned the distinction of being counted among the best stroke care hospitals.
Welcome Onboard
 Dr. Arya Suchismita
Dr. Arya Suchismita
Consultant - Paediatric
Gastroenterology and Hepatology
Medanta - Patna
Paediatric gastroenterologist and hepatologist with expertise in diagnosis and management of causes of pain in abdomen, vomiting, chronic liver disease like Wilson’s disease, autoimmune hepatitis, PFIC, etc. She specialises in all types of diagnostic and therapeutic endoscopies of the upper and lower GI, including endoscopic removal of foreign body, variceal sclerotherapy, band ligation / APC / haemorrhoidal sclerotherapy, in addition to polypectomy for management of upper and lower GI bleeding.
 Dr. Mohan Lal Sharma
Dr. Mohan Lal Sharma
Consultant - Internal Medicine
Medanta - Gurugram
Physician with expertise in managing fevers, tropical disease, pyrexia of unknown origin, lifestyle disorders, urinary tract infections, headache, epilepsy, stroke and multisystem diseases.
 Dr. Anurag Verma
Dr. Anurag Verma
Consultant - GI Surgery, GI Oncology
and Bariatric Surgery
Medanta - Lucknow
Gastrointestinal surgeon with expertise in advanced laparoscopic surgery, failed laparoscopy and open surgery, complex gastrointestinal surgery, complex hernia surgery and bariatric surgery.
 Dr. Anuj Dhyani
Dr. Anuj Dhyani
Associate Consultant - Paediatric
Critical Care
Medanta - Gurugram
Critical care expert with expertise in management of critically ill paediatric patients on ventilators, managing children on extracorporeal device like CRRT and ECMO, in addition to performing paediatric functional ECHO, intubation, ultrasound-guided central lines, arterial lines and haemodialysis catheters.
 Dr. Suman Kumar
Dr. Suman Kumar
Associate Consultant - Institute of
Critical Care and Anaesthesiology
Medanta - Patna
Anaesthesiologist with expertise in administering general anaesthesia, regional anaesthesia, paediatric and neuro anaesthesia, in addition to ultrasound guided nerve block and central venous cannulation.
 Dr. Neha Kumari
Dr. Neha Kumari
Associate Consultant - Dermatology
Medanta - Patna
Dermatologist with expertise in clinical dermatology, dermatosurgery, aesthetics, laser procedures, paediatric dermatology, dermato-rheumatology, hair and nail disorders, and sexually transmitted diseases.






