THE EXCHANGE | Newsletter - Feb 2023
A Knowledge Sharing Initiative by Medanta
Medanta Enhances its Urological Expertise
Appoints Leading Surgeon Dr. Gagan Gautam and Team to
Further Strengthen its Robotic Uro-Oncology Surgery Program

Expanding its pool of clinical experts who deliver holistic, advanced healthcare, Medanta has
appointed renowned robotic uro-oncological surgeon Dr. Gagan Gautam as Vice-Chairman of Uro-
Oncology and Robotic Surgery. Dr. Gautam and his team of robotic surgery specialists - Dr. Puneet
Ahluwalia (Director) and Dr. Gopal Sharma (Consultant) - have joined Medanta’s accomplished
clinicians at the Kidney and Urology Institute, led by Group Chairman Dr. Rajesh Ahlawat. At the
forefront of delivering cutting-edge treatments, the institute is one of the highest-volume robotic
kidney transplant centers in India and is known for its exceptional success rate in robotic and
laparoscopic uro-oncology procedures.
An accomplished robotic surgeon, Dr. Gautam has over two decades of experience in treating
cancers of the urinary system, including kidneys, bladder and prostate gland. Him and his team have
done over 1,500 robot-aided uro-oncological surgeries, and specialise in robotic prostatectomy,
robotic partial nephrectomy and robotic cystectomy.
The team will further strengthen Medanta’s collaborative approach of providing end-to-end
diagnosis and treatment of urinary cancers with its extensive experience in minimally invasive
(robotic and laparoscopic) and open surgeries, development of new treatment techniques, and
initiating and developing urological robotic surgery programs all over the country.
“Appointment of senior doctors like Dr. Gagan Gautam and team is in line with our commitment to
always deliver the highest standard of care by expanding our team of accomplished doctors.
Strengthening our clinical leadership, we welcome Dr. Gautam and team to the Medanta family.”
Dr. Naresh TrehanChairman & Managing Director, Medanta
Medanta@Work
India’s First Simultaneous Three-Way Paired Exchange Liver Transplant without Non-Directed Donation
Novel Strategy to Expand the Donor Pool
ABO (blood group) incompatibility, donor liver steatosis (fatty liver) and low graft-to-recipient body
weight ratio (GRWR) - inadequate volume of partial liver graft from living donor - are the most
common reasons for living donors getting rejected for living donor liver transplantation (LDLT). Apart
from ABO-incompatible liver transplants, and dual lobe LDLT - wherein partial livers are taken from
two donors and transplanted in the recipient - the problems of blood group incompatibility and low
GRWR can be overcome with paired exchange LDLT (PE-LDLT).
In 2009, the Medanta Liver Transplant Team introduced the concept of living donor organ swap (or
paired exchange) between two recipient-donor pairs. Such exchanges help save lives of recipients
whose relatives, despite being medically fit, are unable to donate due to blood group and/or liver
size incompatibility.
In India, the Human Organ Transplantation Act does not permit non-directed donation, and allows
PE-LDLT only between recipient-donor pairs who are spouses or first-degree relatives. After
performing 46 such two-way swaps (92 transplants) over 13 years, the Medanta Liver Transplant Team

successfully performed the country’s first three-way liver transplant swap without a non-
directed donor recently. Three patients suffering from terminal liver disease received life-saving liver
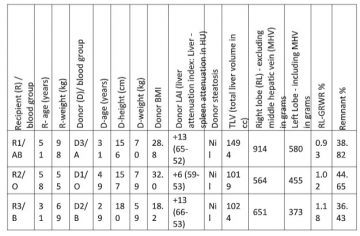
transplants simultaneously. Two recipient-donor pairs participated to overcome ABO
incompatibility, while in the third pair (recipient AB / donor O blood groups) the estimated GRWR
with the right lobe was too low (0.57%), but was adequate for another recipient who sought a blood-
group matched donor.
Concept
As shown in the figures below, a three-way, or longer, PE chain can be initiated in LDLT by a
recipient-donor pair wherein the recipient’s blood group is AB or the donor’s is O (or both), the
estimated GRWR is too low, but adequate for another recipient who seeks a blood-group matched
donor.
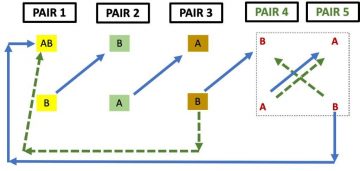
In this example, the paired exchange chain starts with pair 1, with
recipient and donor of blood groups AB and B, respectively, where the
estimated GRWR is low. It can involve five recipient-donor pairs (blue
arrow option), or may stop at three, and the fourth and fifth pairs can
participate in a separate two-way swap (green dashed arrow option).
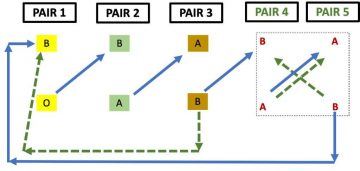
In this example, the paired exchange chain starts with pair 1, with
recipient and donor of blood groups B and O, respectively, where the
estimated GRWR is low. It can involve five recipient-donor pairs (blue
arrow option), or may stop at three, and the fourth and fifth pairs can
participate in a separate two-way swap (green dashed arrow option).
While longer than three- or four-way chains are logical when Good Samaritan donors initiate it and
one of the recipients does not have a live donor, they are often not needed in PE-LDLT. In this case,
all recipients contributed a donor to the exchange, and no non-directed donor was involved.
All recipients underwent pre-transplant evaluation, including assessment of severity of liver disease,
and detailed systemic, psychiatric, and dietetic assessment. All donors also underwent detailed liver
assessment with triphasic contrast enhanced CT scan. Prior to transplant, all LDLTs in India require
an Ethics Committee (Authorization Committee) clearance, which was duly obtained for this triple
swap as well.
Post-transplant, recipients were managed on triple immunosuppression with tacrolimus,
mycophenolate and steroids, and were administered prophylactic antibiotics for five days and
fluconazole for 14 days.
Issue 59February 2023
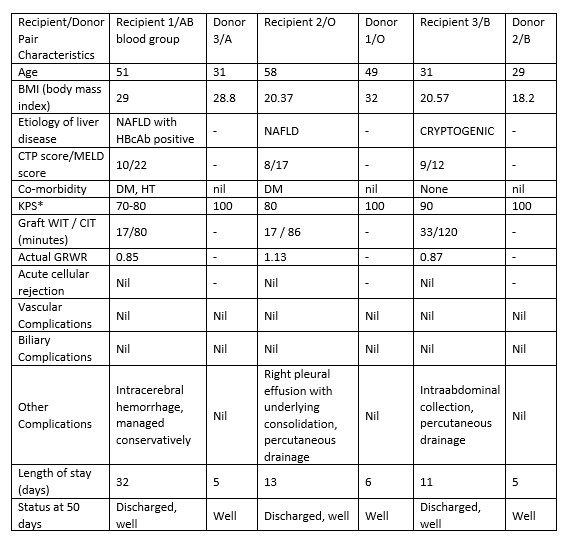
to simultaneously manage three LDLTs peri-operatively. Having previously performed three LDLTs on
the same day a few times, we felt we were adequately equipped, and hence proceeded with it.
In future, simultaneous inter-center PE-LDLTs between experienced, large-volume centers within the
same city could be envisaged, using mutually acceptable management protocols. Towards this, the
regulatory procedure for these LDLTs needs to be defined.
Dr. Prashant Vilas Bhangui
Associate DirectorInstitute of Liver Transplantation and Regenerative Medicine
Medanta – Gurugram
Dr. Amit Nath Rastogi
DirectorInstitute of Liver Transplantation and Regenerative Medicine
Medanta – Gurugram
Dr. Narendra Singh Choudhary
Senior ConsultantInstitute of Liver Transplantation and Regenerative Medicine
Medanta – Gurugram
Dr. Neeraj Saraf
Senior Director - HepatologyInstitute of Liver Transplantation and Regenerative Medicine
Medanta – Gurugram
Dr. Arvinder Singh Soin
ChairmanInstitute of Liver Transplantation and Regenerative Medicine
Medanta – Gurugram
TechByte
Medanta Pioneers
Advanced TAVI Technique
New Technology Offers Hope to Patients with Narrow Vessels
Dr. Praveen Chandra, the Chairman of Interventional Cardiology at the Heart Institute in Medanta -
Gurugram has performed India’s first Transcatheter Aortic Valve Implantation (TAVI) using the newly
launched Evolut Pro+ TAVI technology - an advancement of the existing TAVI technologies to treat
severe symptomatic aortic stenosis. The complex implantation was done recently for a 65-year-old
patient suffering from severe aortic stenosis.
Calcific aortic stenosis - the most common valvular heart disease - is a major public health burden.
TAVI is a novel procedure that brings hope to those suffering from severe aortic stenosis, which
narrows the aortic valve acutely causing breathlessness and fatigue. The disease limits everyday
activities of patients and worsens rapidly.
Unlike surgical aortic valve replacement, which requires a long incision down the chest (open-heart
surgery), TAVI is a minimally invasive procedure done using a thin, flexible tube (catheter) passed
through a few small incisions to reach the heart. The patient’s hospital stay, pain and chances of
complications are minimized with this latest transcatheter technique to replace aortic valve. The
new technology helps optimize procedural outcomes and future access.
Evolut Pro+ is a self-expanding valve made of nitinol frame and porcine pericardial tissues. Nitinol is
an alloy that can be crimped in cold solution and once it comes up to normal temperature, through
contact, it expands to its previous shape. A catheter with crimped valve is inserted into femoral
artery, and guides the valve into the heart. Moving X-ray images in Cath Lab help the doctor place
the catheter to the correct position. The catheter is removed once the new valve is securely
deployed in place.
The next generation Transcatheter Aortic Valve System provides top notch safety and is a
recapturable system, hence it can be retrieved and repositioned to achieve best results. This new
system offers the lowest delivery profile for 23-29 mm valves, excellent hemodynamics allowing
patients to return to activity sooner, the broadest annulus range, and advanced sealing with an
external tissue wrap on all valve sizes.
With a reduced delivery profile for 23-29 mm valves, it is indicated to treat patients with vessels as
small as 5.0 mm. With the ability to treat the broadest annulus range of any other available TAVI
system, these new valves can treat annulus ranges from 18 mm to 30 mm.
Dr. Praveen Chandra

Chairman Interventional and Structural Heart CardiologyHeart Institute
Medanta – Gurugram
In Focus
Deep Brain Stimulation to Treat Drug-Resistant Epilepsy in 7-year-old
Epilepsy is a common neurological problem in India. However, with advancements in investigations
and medicines, the disease is manageable in majority of the cases. About two-thirds of all epilepsy
patients exhibit good control over symptoms and disease progression with medication. However,
the remaining one-third continue to experience seizures despite medication, and come under the
category of patients with drug-resistant epilepsy.
Management of drug-resistant epilepsy requires a comprehensive workup, including a special
epilepsy protocol involving use of magnetic resonance imaging (MRI) and video
electroencephalography (EEG) of the brain to identify the root cause. If a clear focal point is found in
the brain, which is responsible for these seizures, an epilepsy surgery can be done offering excellent
outcome at centres with experienced surgeons. But, in some patients, no such foci are found despite
extensive workup, including MRI, video EEG or positron emission tomography (PET) scan, etc.
However, satisfactory improvement can be achieved in such patients with the use of stimulation
techniques including Deep Brain Stimulation (DBS) and Vagal Nerve Stimulation (VNS). Here, we
discuss the case of a young girl with recurrent seizures since childhood.
Case Study
A 7-year-old girl presented at Medanta - Gurugram with a history of recurrent seizures since 10
months of age. All her seizures were grand mal seizures – involving loss of consciousness and violent
muscle contractions lasting for 2-3 minutes followed by prolonged confusion in the recovery phase.
Her seizures were frequent, with one to two episodes being reported in a week. The patient was
born after a full-term, normal delivery with age-appropriate developmental milestones. She did not
have a history of head injury or any family history of epilepsy. The patient was on multiple anti-
epileptic drugs without significant improvement in her condition.
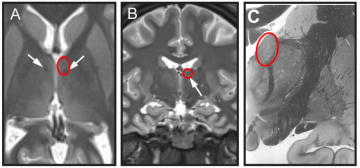
The patient was worked up in detail for drug-resistant epilepsy using clinical assessment followed by
MR imaging and video EEG. Using video EEG, her seizures were recorded and correlated with EEG
changes at the time. This helped in diagnosing the type of epilepsy she suffered from. However, we
could not establish a single focal point of origin, and multiple areas showed abnormal firing or
spikes.
Her MRI brain epilepsy protocol was done, and it only showed diffused brain atrophy in view of non-
localization of epilepsy. PET-CT brain was also done which showed diffused hypometabolism in
bilateral temporal, parietal and left occipital lobes. Overall, the MRI and PET scan indicated that the
brain was significantly abnormal at multiple points.
No clear seizure foci could be found indicating diffused brain changes and hence epilepsy surgery to
remove such foci was not feasible. Such cases of diffused brain damage with drug-resistant epilepsy
pose significant challenge for the treating neurologists. They remain a major cause of morbidity for
majority of the population suffering from epilepsy.
Earlier done for managing movement disorders, DBS is now being done for intractable drug-resistant
epilepsy targeting various cortical and subcortical structures. For the procedure, very thin electrodes
are placed deep in the brain to stimulate certain parts. But electrode placement in cases of
childhood epilepsy can be challenging as the targeted area is ventral thalamus – a crucial area of the
brain surrounded by numerous critical nuclei and white matter tracts in addition to ventricles. Even
the smallest error in the trajectory can cause significant morbidity, besides leading to sub-optimal
outcomes.
Our patient underwent DBS targeting bilateral thalami. To control the seizure frequency, two
trajectories were planned - tranventricular and subcaudate paraventricular. Target was the anterior
nucleus of the thalamus (ANT). The anterior nucleus of the thalamus is used as target for limbic
seizure disruption. It is around 4x10x5.5 mm in size and located at the floor of the lateral ventricles
surrounded by the choroid plexus, thalamostriate vein and the internal cerebral veins. In our case,
we used the right side tranventricular trajectory to hit the sweet spot, and for the left side we used
paraventricular trajectories as shown in the images.
After careful planning and submillimeter checks, the electrodes were placed in the brain by
tranventricular and subcaudate trajectories under neuro-navigation guidance. The surgery was
uneventful with good clinical outcome. In the post-operative period, the patient regained
consciousness on the same day. She was shifted to room on Day 1 of surgery and was discharged on
Day 3 in stable condition. During her post-operative hospital stay, she did not have any seizures.
On her one-month post-operative follow up as well, the child was doing well and did not report having
any major seizures. Initial results for DBS in epilepsy treatment were promising in this case and we
expect it to offer good control of seizures in the long run.
DBS has emerged as a safe and effective treatment modality for the management of drug-resistant
epilepsy non-amenable by surgery showing excellent results.
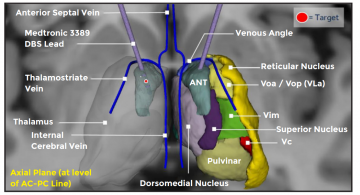
3D representation of the thalamic nuclei and the target superimposed on the axial MRI
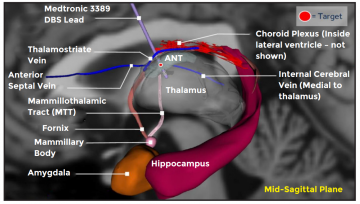
Sagittal MRI with anatomy
Medanta-Gurugram is pioneer in DBS surgery for epilepsy in India and has done four such
procedures after extensive patient evaluation for optimal outcome.
Dr. Atma Ram Bansal
Associate Director - Epilepsy ProgrammeInstitute of Neurosciences
Medanta – Gurugram
Dr. Sudhir Dubey
Chairman - Endoscopic Portal Minimal Invasive NeurosurgeryInstitute of Neurosciences
Medanta – Gurugram
Welcome on board
Dr. Praveen Khilnani
Chairman – Paediatrics, Paediatric Pulmonology and Paediatric Critical Care
Medanta – Gurugram
Paediatric critical care specialist and pulmonologist with nearly four decades of experience and
expertise in paediatric ventilation, neonatal and paediatric bronchoscopy, pulmonary asthma,
childhood allergies, chest diseases and chronic illnesses from birth till 18 years of age.
Dr. Gagan Gautam
Vice ChairmanUro-Oncology and Robotic Surgery
Medanta – Gurugram
Pioneer of robotic surgery in India with over two decades of experience in the surgical treatment of
urological cancers. His areas of expertise include robotic prostatectomy, robotic partial nephrectomy
and robotic cystectomy.
Dr. Rajiv Ranjan Prasad
Director - Radiation Oncology
Medanta – Patna
Radiation oncologist with over 30 years of experience and expertise in treating breast cancer, gastro
intestinal cancers, urogenital cancers and cancers of the central nervous system.
Dr. Rajiv Uttam
Director and Head of Department Paediatrics, Paediatric Intensive Care Unit and Paediatric
Emergency
Medanta – Gurugram
Paediatric critical care specialist and pulmonologist with nearly four decades of experience and
expertise in paediatric ventilation, neonatal and paediatric bronchoscopy, pulmonary asthma,
childhood allergies, chest diseases and chronic illnesses from birth till 18 years of age.
Dr. Rajiv Ranjan Prasad
Director - Radiation Oncology
Medanta – Patna
Radiation oncologist with over 30 years of experience and expertise in treating breast cancer, gastro
intestinal cancers, urogenital cancers and cancers of the central nervous system.
Dr. Puneet Ahluwalia
Director and Head Uro-Oncology and Robotic Surgery
Medanta – Gurugram
Uro-oncologist with expertise in robotic surgeries for treating urological cancers. He specialises in
radical prostatectomy, partial nephrectomy, radical cystectomy, adrenalectomy, retroperitoneal
lymph node dissection and video endoscopic inguinal lymph node dissection (VEIL).
Dr. Kishore Jhunjhunwala
Director - Critical Care
Medanta – Patna
Intensivist with expertise in managing critically ill patients. He specialises in extracorporeal therapy,
haemodynamic monitoring, mechanical ventilation and managing difficult airway.
Dr. Roma Pradhan
Associate DirectorEndocrine and Breast Surgery
Medanta – Lucknow
Endocrine and breast surgeon with expertise in breast surgery (benign and cancerous), oncoplastic
breast cancer surgery, thyroid cancer surgery, adrenal and parathyroid surgery besides diabetic foot
management.
Dr. Gopal Sharma
ConsultantUro-Oncology and Robotic Surgery
Medanta – Gurugram
Uro-oncologist with expertise in management of urological cancers including prostate, kidney and
bladder. He is a trained robotic surgeon.
Dr. Resham Srivastava
Senior Consultant - Radiation Oncology
Medanta – Lucknow
Radiation oncologist with expertise in image-guided radiation therapy (IGRT), intensity-modulated
radiation therapy (IMRT), volumetric modulated arc therapy (VMAT), stereotactic body radiation
therapy (SBRT), stereotactic radiation therapy (SRT) and brachytherapy.
Dr. Gaurav Bharadwaj
Consultant - Liver Transplant Surgery
Medanta – Lucknow
Gastrointestinal surgeon with expertise in hepato-pancreato-biliary malignancies, redo surgeries and
advanced laparoscopic surgeries for GI malignancies.
Dr. Neeraj Bharti
Consultant - Internal Medicine
Medanta – Patna
Physician with expertise in managing and treating infectious diseases, such as COVID-19, and non-
infectious lifestyle diseases including diabetes, hypertension and thyroid disorders.
Dr. Gaurav Kumar
Consultant - GI Surgery, GI Oncology and Bariatric Surgery
Medanta – Patna
Gastrointestinal surgeon with expertise in advanced laparoscopic surgeries, especially of cancers of
the upper and lower gastrointestinal systems. He specialises in laser proctology, laparoscopic colorectal surgery and hernia surgery including laparoscopic cholecystectomy appendectomy, and hepatobiliary surgeries.
Satish Kumar Ranjan
Associate ConsultantUrology and Kidney Transplant Surgery
Medanta – Patna
Urologist with expertise in treating urological problems in patients of all ages. He specialises in endourology, uro-oncology, andrology and kidney transplantation.






