Heart Palpitations: Why They Happen & How to Stop Them

TABLE OF CONTENTS
That fluttering, pounding, or racing sensation in your chest? These heart palpitations are more common than you might think. Research shows that many people ask their primary care doctors about these unsettling sensations. These symptoms are one of the main reasons patients book appointments with cardiologists.
Your heart typically beats between 60 to 100 times per minute. Sometimes this rhythm gets disrupted and you become aware of heartbeats that usually go unnoticed. These palpitations might feel scary, but they are nowhere near as dangerous as they seem. Many factors can trigger or make them worse—from everyday stress to your evening glass of wine. Studies link even modest alcohol consumption to a higher risk of certain heart rhythm problems.
You might wonder when these unusual heart sensations become a real concern. These symptoms are common, but they can sometimes point to heart conditions that need medical attention. The good news? If your heart is healthy, most cases don't need any treatment. This article explains why it happens, when you should worry, and gives you practical ways to handle palpitations both right now and in the future.
What Are Heart Palpitations?
Your heart beats out of rhythm when an electrical signal fires from the wrong place at the wrong time - this causes palpitations. A healthy heart beats 60-100 times per minute. The sensation of discomfort in your chest makes more sense once you understand what happens during these episodes. Heart palpitations show themselves when you become aware of your heartbeat. Your heart might race, pound, flutter, or skip beats. These sensations might show up in your chest, throat, or neck.
People often notice what seems like a "skipped" beat, but it's actually an early heartbeat. The ventricles don't have enough time to fill with blood, so little or no blood gets pumped out. This creates that skipping feeling. The next beat feels stronger because it pumps out extra blood volume.
What are the Causes of Heart Palpitations in Adults?
Several factors can trigger these unsettling sensations:
Emotional triggers: Stress, anxiety or panic attacks
Lifestyle factors: Caffeine, alcohol, nicotine or recreational drugs
Physical conditions: Strenuous exercise, fever, dehydration
Medical issues: Thyroid problems, anaemia, low blood sugar
Hormonal changes: Pregnancy, menstruation, menopause
Medications: Asthma inhalers, decongestants, diet pills
Signs That Palpitations Could Indicate Heart Disease
Palpitations are usually harmless. However, you should seek medical help right away if you experience chest pain, shortness of breath, dizziness, unusual sweating, or fainting along with palpitations.
You should also contact your doctor if palpitations happen frequently (more than 6 per minute or in groups of 3+), if you have existing heart disease, or if your pulse goes above 100 beats without exercise.
Managing Palpitations Naturally and Medically
Deep breathing techniques help manage palpitations naturally.
Staying hydrated, identifying and avoiding triggers, and reducing stress through yoga or meditation can make a difference.
Vagal manoeuvres like forceful coughing or splashing cold water on your face can help regulate your heart rate.
Tests Cardiologists May Recommend
Medical history and physical assessment: Your doctor will ask about your symptoms and check your pulse, blood pressure and listen to your heart and lungs to know the reason for the heart palpitations.
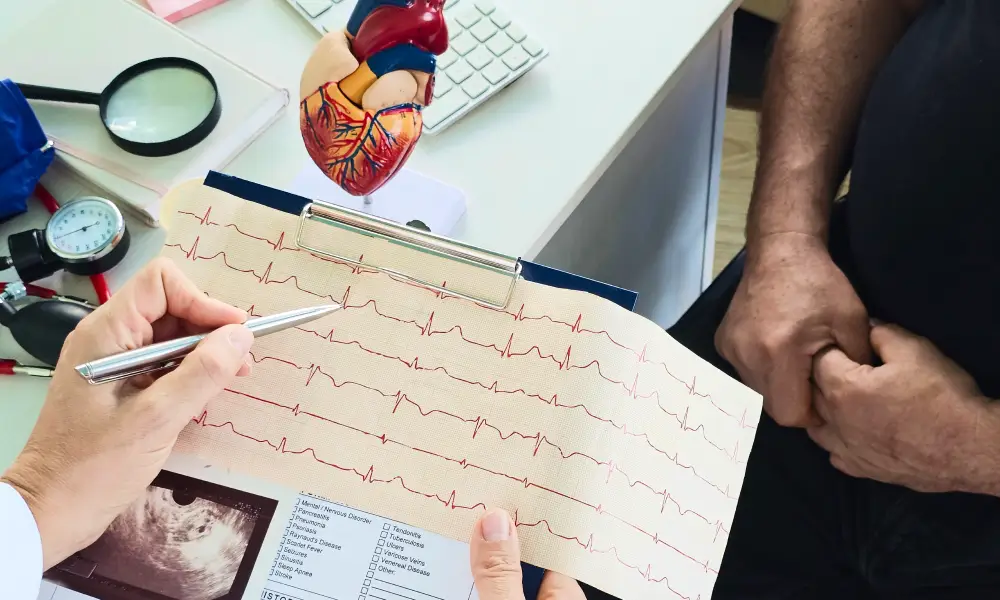
Electrocardiogram (ECG): Records your heart's electrical activity to detect abnormal rhythms
Holter monitoring: You wear a small device for 24-48 hours to monitor how your heart beats and to catch any unusual patterns.
Echocardiogram: This heart ultrasound examines your heart's structure, motion and function
Blood tests: To rule out other diseases that could cause palpitations like thyroid imbalance, anaemia, or electrolyte disturbances
Treatment
The treatment plan depends on what's causing the palpitations. Options are:
Lifestyle changes:
Reduce caffeine and alcohol consumption
Lower your stress levels
Take at least 7-8 hours of sleep
Identify and avoid your palpitations' triggers
Medications: Doctors sometimes recommend medicines such as beta-blockers or calcium channel blockers that control heart rhythm.
Treating medical issues: Doctors will tailor your treatment to manage underlying conditions, such as thyroid medicines or treatment of anaemia.
Conclusion
Heart palpitations can be scary, but they affect many people and rarely indicate serious problems. You can manage these unsettling sensations better once you identify your personal triggers. Stress, caffeine, or normal hormonal changes cause most cases rather than dangerous heart conditions.
Your body will tell you when you need medical attention through warning signs like chest pain, dizziness, fainting, or shortness of breath with palpitations. These signals clearly show when professional care is needed. Simple strategies work well for most people in other situations.
You can reduce episodes substantially by breathing deeply, staying hydrated, and avoiding known triggers. On top of that, vagal manoeuvres are a great way to get quick relief during uncomfortable moments. Lifestyle changes help most people, but doctors can suggest more options through testing and medication if needed.
The most valuable lesson is this: being aware of your heartbeat doesn't mean danger. Your body sometimes makes normal functions more noticeable without any real cause for concern.
FAQs
When should I worry about palpitations?
Get medical help right away if you have palpitations with:
Chest pain or discomfort
Severe shortness of breath
Dizziness or light-headedness
Fainting or blackouts
Unusual sweating
You should also call your doctor if your palpitations get worse or happen more often. The same goes if your pulse is faster than 100 beats per minute without exercise. Any palpitations that last more than a few minutes need medical attention.
Do palpitations mean heart failure?
Most palpitations don't signal heart failure, but there can be a connection. People who have heart failure might feel their heart racing as it tries to make up for weaker pumping. Some irregular heartbeats can reduce your heart's pumping power. This could lead to heart failure if you don't treat it. So while most palpitations are harmless, you should get persistent ones checked out.
Can dehydration cause heart palpitations?
Yes, it can. Your heart works harder to pump blood that's too thick from dehydration, which makes it beat faster. A lack of fluids throws off your body's electrolyte balance and affects your heart's electrical system. You might notice other signs too - dark urine, dizziness, headaches, and feeling unusually tired. The good news is that drinking water or sports drinks usually fixes these palpitations quickly.
Are palpitations common in anxiety?
Anxiety tops the list of non-heart-related causes of palpitations. Your body kicks into fight-or-flight mode during anxious moments, releasing stress hormones that speed up your heartbeat. About one in five people deal with anxiety disorders at some point. The symptoms often feel like a heart attack, which makes many people panic even more.
Is an ECG enough to detect an irregular heartbeat?
An ECG helps, but it can't catch everything. It only records about 12 seconds of heart activity, so it might miss irregular beats that come and go. Your doctor might suggest wearing a portable monitor if your palpitations happen occasionally. These include Holter monitors for 24-48 hours or event monitors for about 30 days. The devices you can activate yourself work great to connect your symptoms with your actual heart rhythm.






