Atrial Fibrillation: Types, Causes & Modern Treatment Options
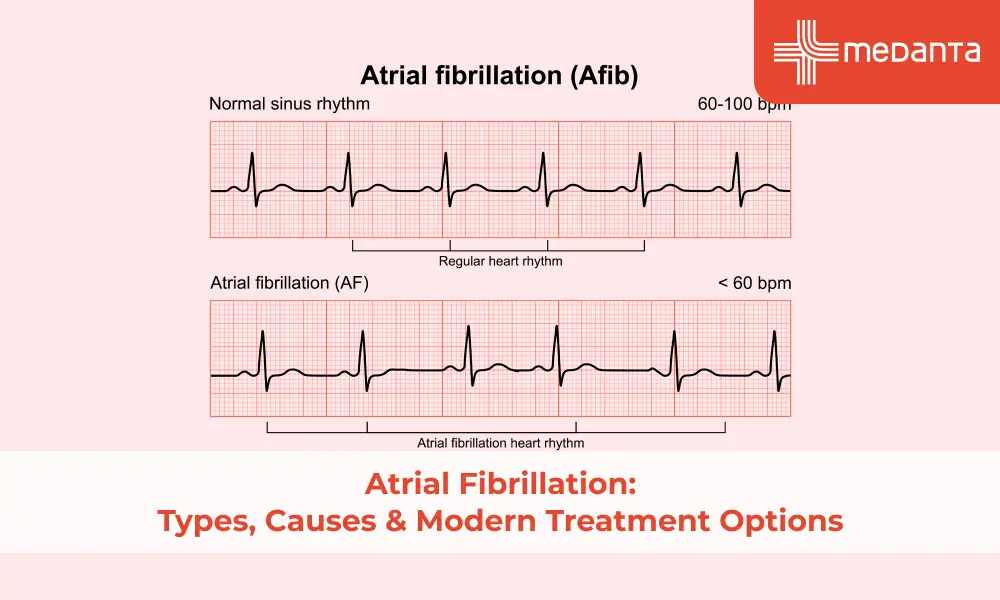
TABLE OF CONTENTS
- What Is Atrial Fibrillation (AFib)?
- Common Causes of Atrial Fibrillation
- Risk Factors That Trigger AFib
- Symptoms of Atrial Fibrillation You Shouldn't Ignore
- How AFib Affects Your Heart and Health
- AFib vs. Normal Irregular Heartbeat: What's the Difference?
- When to Seek Medical Help for Atrial Fibrillation
- Diagnosis: How AFib is Detected
- Modern Treatment Options for Managing Atrial Fibrillation
- Conclusion
- FAQs
Millions of people worldwide deal with atrial fibrillation, and treatment options keep getting better. Atrial fibrillation (AFib) stands as the most common heart rhythm disorder. This irregular heartbeat happens when the heart's upper chambers beat out of sync with the lower chambers, which disrupts normal blood flow. People can live with this condition, but AFib patients have a stroke risk that's five times higher than those without it. Patients experience several symptoms that include palpitations, fatigue, breathlessness, and dizziness. The condition comes in four distinct types based on how long episodes last: paroxysmal, persistent, long-standing persistent, and permanent. These types differ mainly by the duration of irregular heartbeat - some patterns fix themselves and others need medical help. Medical advances have made AFib management easier than before, and patients now have more options to keep their hearts healthy.
What Is Atrial Fibrillation (AFib)?
Your heart's upper chambers (atria) beat irregularly instead of maintaining a normal rhythm in atrial fibrillation. The atria quiver rather than contract well, and this makes blood pool. Blood flow gets disrupted by this chaotic electrical activity, which can form dangerous clots. AFib is the most common heart arrhythmia that doctors treat.
Common Causes of Atrial Fibrillation
Here's what typically causes AFib:
Heart tissue or electrical system damage
High blood pressure (causes about 1 in 5 cases)
Heart disease (valve problems, heart failure)
Thyroid disorders (especially with hyperthyroidism)
Sleep apnea
Risk Factors That Trigger AFib
These factors can increase your AFib risk:
Age (risk goes up after 65)
Obesity
Alcohol consumption
Smoking
Existing heart conditions
Family history
Physical inactivity
Symptoms of Atrial Fibrillation You Shouldn't Ignore
Doctors often find AFib during routine check-ups because some people don't show any symptoms. People with AFib often experience:
Irregular heartbeat or palpitations
Fatigue and weakness
Shortness of breath
Dizziness or lightheadedness
Chest pain or pressure
Limited exercise capacity
How AFib Affects Your Heart and Health
AFib doubles your death risk and makes strokes five times more likely. Your heart can't pump blood well with irregular beats. This leads to:
Blood clots that might cause strokes
Heart failure from weakened heart muscle
Poor blood flow to vital organs
Cognitive decline and dementia
AFib vs. Normal Irregular Heartbeat: What's the Difference?
Feature | Atrial Fibrillation | Normal Irregular Heartbeat |
Pattern | Completely chaotic rhythm ("irregularly irregular") | May follow patterns (e.g., every third beat feels off) |
Duration | Can be persistent or permanent | Often brief and fixes itself |
Stroke Risk | This is a big deal as it means that | Usually not higher |
Blood Thinners | Usually needed | Not needed |
Atrial Movement | Fibrillation (quivering) instead of contraction | Normal contraction with timing changes |
When to Seek Medical Help for Atrial Fibrillation
Get medical help right away if:
You have your first AFib episode
Your resting heart rate goes above 120 beats per minute
You notice stroke signs (face drooping, arm weakness, speech problems)
You feel chest pain, severe breathing problems, or faintness
Note that regular check-ups are crucial because even AFib without symptoms raises your stroke risk.
Diagnosis: How AFib is Detected
Doctors need specific tests to spot heart rhythm patterns in AFib patients. The process starts with a physical exam where doctors check the pulse, blood pressure, and listen to heart sounds. Several diagnostic tests help confirm AFib:
Electrocardiogram (ECG/EKG): This key test records the heart's electrical activity and shows irregular rhythms typical of AFib
Portable monitors: These help track occasional episodes:
Holter monitors track continuously for 24-48 hours
Event recorders capture heart activity for up to 30 days
Implantable loop recorders can monitor for up to three years
Echocardiography: Sound waves create heart images that show its structure and function, which helps spot possible complications
Blood tests also help identify conditions like thyroid disorders or electrolyte imbalances that might set off AFib.
Modern Treatment Options for Managing Atrial Fibrillation
The treatment's main goal is to prevent blood clots, control heart rate/rhythm, and tackle why it happens. Today's treatment approaches include:
Medications:
Blood thinners (anticoagulants): These prevent strokes and blood clots. Patients can take warfarin or newer direct-acting oral anticoagulants (DOACs)
Rate control medicines: Beta blockers, calcium channel blockers, and digoxin help bring down rapid heart rates
Rhythm control medicines: These bring back and keep a normal heart rhythm
Procedures:
Cardioversion: Low-energy electrical shocks or medications help restore normal rhythm.
Catheter ablation: This destroys tissue that causes irregular signals.
Left atrial appendage closure: This stops clots from forming in the heart's small chamber sac
Advanced options include the Maze procedure that blocks abnormal signals with scars, and pacemaker implantation. Weight management and cutting back on alcohol are also key parts of a comprehensive treatment plan.
Conclusion
Atrial fibrillation ranks as one of the most common and serious heart conditions worldwide.
AFib comes in different types - paroxysmal, persistent, long-standing persistent, and permanent. This knowledge helps patients identify their condition better. The symptoms can vary a lot. Some people feel obvious signs like palpitations and fatigue. Others only find out about their condition during regular check-ups.
Medical science has made great progress in managing AFib. Quick diagnosis is vital to make treatment work. People should seek medical help right away if they notice unusual heart rhythms or worrying symptoms. Even AFib without symptoms needs proper care to stop serious complications.
AFib treatment works best with an integrated approach. Medical treatments work, among other changes, like managing weight, limiting alcohol and staying active. AFib brings challenges, but most patients can live well with proper care. Success comes from working closely with doctors to create a customised plan that fits each patient's needs and risks.
FAQs
What is atrial fibrillation and how serious is it?
Atrial fibrillation occurs when your heart's upper chambers beat chaotically and don't sync with the lower chambers. This condition is the most common type of cardiac arrhythmia. AFib can be dangerous because:
Your risk of stroke becomes five times higher than that of people without AFib
You might develop blood clots, heart failure and cognitive problems
The death risk doubles compared to people with normal heart rhythms
What are the main causes of atrial fibrillation?
AFib develops due to several factors:
Damage to the heart tissue or its electrical signalling system
Heart conditions like valve disease and heart failure
High blood pressure
Thyroid problems, especially an overactive thyroid
Sleep apnea
Age-related changes in heart tissue
3. Can stress or anxiety cause AFib?
Stress and anxiety can trigger AFib episodes, and this works both ways:
Your sympathetic nervous system activates with stress, which can trigger AFib
Anxiety lowers heart rate variability and vagal tone, creating perfect conditions for AFib
Your heart tissue can get damaged over time from stress hormones
The condition itself often makes you more anxious, which creates a tough cycle
What does AFib feel like in the chest?
People experience AFib differently, but common sensations include:
A fluttering or "fish flopping" feeling in the chest
Pounding or thumping sensations
Sudden racing heartbeat
Skipped or irregular beats
Pressure or discomfort in the chest
How is AFib different from a heart attack?
These conditions share some symptoms but are fundamentally different:
AFib affects your heart's electrical system, causing irregular rhythm
Heart attacks happen when blood can't flow to the heart muscle
You'll mainly feel palpitations and tiredness with AFib
Heart attacks usually cause pain in your arms, jaw, or back with nausea
You need immediate emergency care for a heart attack
Can atrial fibrillation go away on its own?
Sometimes AFib resolves without treatment:
Paroxysmal AFib episodes stop by themselves within 7 days
You might experience spontaneous remission, but it's rare
Paroxysmal AFib usually progresses to persistent forms without treatment
About 10-20% of paroxysmal cases become persistent AFib within a year






