5 Ways Diabetes Can Affect Your Eyes & Vision
Diabetes is India’s fastest growing health condition, with over 72 million reported cases. The prevalence of diabetes has increased by 64% across India over the last 25 years and is expected to double by 2025.
There are approximately 8 million people in India who have vision impairments, and 80% of these eye-related conditions are curable or preventable. However, visual impairment due to diabetes-related eye disease is the leading cause of blindness in the age group between 20 and 55 years.
How Does Diabetes Affect Your Eyes?
Diabetes is a complex metabolic disease in which the pancreas doesn’t produce enough, or any amount of insulin, resulting in excess levels of sugar in your blood. Insulin helps break down sugar (glucose) that provides energy to your body. When your body doesn’t produce enough insulin, it can affect the eye, including the retina, vitreous, lens, and the optic nerve.
When your blood sugar levels are high due to diabetes, it can affect your eyes and vision directly. It can change the fluid levels or cause swelling in the tissues in your eyes, resulting in blurry vision. In the short-term, you may experience blurred vision until your glucose levels are back to normal.
But if your glucose levels continue to remain high for a long period of time, it can damage the blood vessels behind your eyes, leading to fluid or blood leak and swelling. This condition is often diagnosed at the prediabetes stage when your glucose levels are higher than usual, but not high enough to cause damage. These damaged blood vessels are subsequently replaced with new, weak blood vessels that have a chance of bleeding into the centre of your eye, resulting in scarring, or exorbitantly high pressure inside your eyes causing more damage.
Are There Other Diabetes-related Conditions That Can Affect My Vision?
Most serious diabetes-related eye conditions start with damaged blood vessels. Here are some ways diabetes can affect your eyes and vision:
- Blurry Vision: Blurry vision is one of the first warning signs of progressive diabetes-induced vision impairment. Your vision may be blurred due to a fluid leak into the lens, which makes it swell and change shape. This change inhibits your ability to focus, thereby making things appear fuzzy. You may also experience blurry vision when you just start your insulin treatment for diabetes. For most people, however, vision clears out once their blood sugar levels are stabilised.
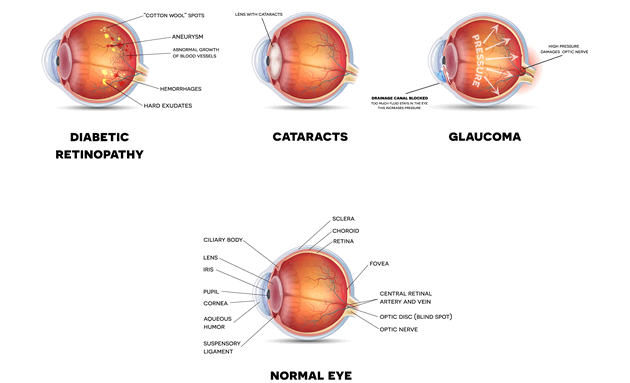
- Cataract: Cataract is the clouding of the lens in your eyes that help you focus, and people with diabetes are more likely to develop them at a younger age. The lens gets oxygen and glucose from the fluid aqueous humour from the front of your eyes. If you’re a diabetes patient, your glucose levels are high which results in swelling of the lens. Furthermore, the lens contains an enzyme Sorbitol dehydrogenase, which if allowed to collect in the lens can affect cells and other proteins, making the lens more opaque and obstructing vision.
- Glaucoma: Glaucoma occurs when the fluid pressure in your eyes are higher than normal. This increased pressure can damage your optic nerve, resulting in vision loss. The longer someone has diabetes, the higher their risks are of developing Glaucoma.
- Diabetic Retinopathy: Retina is a group of cells behind your eyes that are responsible for converting light into signals and send it through the optic nerve to the brain. Diabetic Retinopathy is a condition in which high blood pressure causes your retinal blood vessels to leak fluid or bleed (haemorrhage), resulting in scarring and cell loss in your retina.
Diabetic Retinopathy has 4 stages and 1 worsened condition:
- Mild nonproliferative retinopathy, which is a small, balloon-like swelling in your blood vessels (microaneurysms) and occurs at the earliest stage of the disease
- Moderate nonproliferative retinopathy, the second stage, which may cause blood vessels to lose their ability to transport blood.
- Severe nonproliferative retinopathy, where more blood vessels get blocked, depriving blood supply to parts of the retina that secrete growth factors that signal the retina to grow new blood vessels.
- Proliferative diabetic retinopathy, in which growth factors secreted by your retina triggers the growth of new, weaker blood vessels that are likely to bleed. This can lead to scarring of your tissues and cause retinal detachment (peeling away of the retina from underlying tissues) and result in permanent vision loss.
- Diabetic Macular Edema (DME), is the most common cause of vision loss for people with Diabetic Retinopathy. It is a fluid build-up (oedema) in the macular region of your retina responsible for providing sharp and straight vision. It is most likely to occur as Diabetic Retinopathy worsens.
- Common, mild conditions: Lesser and more common effects of diabetes that you may notice are:
- Headaches
- Eye pain
- Blurry vision
- Watery eyes
- Halos around lights
How Often Does a Diabetes Patient Need to Get an Eye Checkup?
Usually, symptoms don’t show too early, but it’s best to get regular eye-checkups done, especially if you’re a diabetes patient. When symptoms do occur, they may include
- Blurry or wavy vision
- Frequently changing vision—sometimes from day to day
- Dark areas or vision loss
- Poor colour vision
- Spots or dark strings (also called floaters)
- Flashes of light
How Can Diabetics Take Care of Their Eyes?
Follow these steps now to make sure you take care of your vision in the years to come.
- Get a comprehensive eye checkup done by your ophthalmologist at least once a year
- Control your blood sugar levels by following a doctor-advised diet and drinking lots of clear fluids
- Maintain and check your blood pressure and cholesterol levels from time to time
- If you’re a smoker, quit smoking and limit the consumption of alcohol
- Add physical exercise to your daily routine and stay as active as possible
If you’re a patient with diabetes, the good news is that proper care and early detection of any diabetes-induced eye-related conditions can help manage your symptoms and preserve your vision for longer. It is advised to get your share of checkup today.






