THE EXCHANGE | Newsletter - Oct 2023
Total Ablative Radiosurgery in Oligometastatic RCC
Renal cell carcinoma (RCC) is the eighth most common cancer worldwide and accounts for approximately 90% of all kidney malignancies. Both radical nephrectomy (RN) and partial nephrectomy, also known as nephron-sparing surgery (NSS), are accepted as the standard of care. For older patients, particularly those with pre-existing comorbidities, high risk for anaesthesia and chronic kidney disease (CKD), non-surgical treatments are offered, including radiofrequency ablation and cryotherapy. Typically, with such treatments only smaller lesions, located away from the ureter and vascular structures, can be treated because of risks including the heat-sink effect, stricture, fistula development. Safety and effectiveness of stereotactic body radiotherapy (SBRT) has been proven in oligometastatic RCC lesions. SBRT to primary kidney tumour has also been found to be an effective and safe modality, showing excellent oncological outcome in medically inoperable patients with localised cancers regardless of the location and the size of tumour.
SBRT has been recommended as a category-2B treatment option for Stage-1 kidney cancer in the National Comprehensive Cancer Network (NCCN) guideline. Although nephrectomy is practiced in oligometastatic RCC, there are many patients who are medically unfit for surgery and their optimal management unclear. There is scarcity of data on the synchronous delivery of SBRT to primary and oligometastatic sites. We report our experience of synchronous delivery of SBRT to primary RCC and oligometastatic site (brain metastasis), referred to as ‘Total Ablative Radiosurgery’.
Case Study
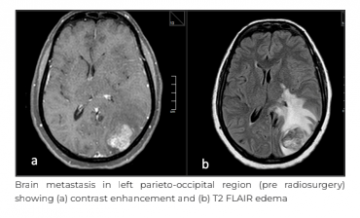
A 64-year-old female with comorbidities, including diabetes and hypertension, presented to Medanta -Gurugram with complaints of headache and one episode of seizure in February 2022. There were no complaints related to motor or sensory deficit, vomiting, bone pain, haematuria, weight loss or fever. On examination, her Eastern Cooperative Oncology Group (ECOG) performance status was 1, with no neurological deficit. Her haemogram, renal and liver biochemistry were within laboratory limits. She was evaluated with contrast magnetic resonance imaging (MRI) of the brain, which showed an oval shaped mass of 22mmx14mm in left parieto-occipital region and another 5mm lesion in left occipital para-sagittal region. Parieto-occipital lesion was hyperdense, heterogeneously enhancing, as seen on contrast images, with well-defined margins, areas of necrosis and mild perilesional oedema. Spectroscopy showed raised choline creatinine ratio. Imaging findings were suggestive of neoplastic aetiology, more in favour of metastasis than primary brain pathology.
She was further evaluated with a whole body positron emission tomography - contrast enhanced computed tomography (PET - CECT) scan, which revealed an enhancing, hyperdense lesion in the left parieto-occipital region, measuring 24mmx15mm with perilesional oedema. Another enhancing, hyperdense lesion was noted in the left occipital para-sagittal region measuring 5mm. An exophytic solid heterogeneously enhancing lesion was arising from the mid pole of the right kidney, measuring 23mmx22mm with heterogeneous fluorodeoxyglucose (FDG) uptake – the maximum standardised uptake value (SUV max) was 6.71 with perilesional fat stranding. It was closely abutting segment six of the liver with loss of fat plane. Imaging findings were suggestive of primary renal neoplastic pathology with brain metastasis.
This was followed by ultrasound - guided (USG) biopsy from the renal mass, which was reported as clear cell RCC. Thus, a diagnosis of RCC with brain metastasis, Stage-4, was made, as per the International Metastatic RCC Database Consortium (IMDC) favourable risk profile.
The patient completed SRS for brain metastasis (2400cGy in three fractions) and SBRT to the rena lesion with a dose of 5000cGy in five fractions in June 2022. She was discharged on anti-epileptics and was adviced review with the Medical Oncology Team for systemic treatment.
The case was discussed by the multidisciplinary tumour board (MDTB) of Medanta - Gurugram comprising of a radiation oncologist, a medical oncologist, uro-oncology surgeons, radiologists and pathologists. The MDTB was of the consensus that the brain metastasis should be treated with stereotactic radiosurgery (SRS) followed by nephrectomy.
After local therapies, the patient was recommended systemic therapy. The MDTB recommendation was discussed with the patient and her family, but the patient did not agree for surgical management and defaulted for three months. She started an alternative therapy and stopped the prescribed anti-epileptics. After three months of the MDTB meeting, she presented with increasing symptoms of headache and a few episodes of seizures.
The MRI brain and PET scan were repeated. They showed increase in size of brain metastasis to 36mmx27mm, while other smaller lesion of 5mm remained stable. The renal lesion also remained stable in size, and the FDG avidity without any evidence of new metastasis.
The patient and her family refused any surgical intervention at the second consult as well. The case was re-discussed with the MDTB and the patient was planned for radiosurgery of brain metastasis and SBRT to kidney tumour followed by systemic therapy.
The patient completed SRS for brain metastasis (2400cGy in three fractions) and SBRT to the renal lesion with a dose of 5000cGy in five fractions in June 2022. She was discharged on anti-epileptics and was adviced review with the Medical Oncology Team for systemic treatment.
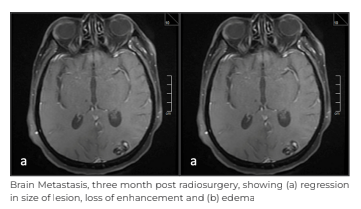

The patient chose not to pursue systemic therapy and returned after three months with PET - CECT scan and MRI brain. There was an interval decrease in the size of the previously seen enhancing, hyperdense lesion in the left parieto-occipital region, now measuring 17mmx10mm against the previous size of 36mmx27mm. Interval decrease was also seen in the surrounding perilesional oedema; smaller brain lesion showed interval.
Two subsequent imaging at six months and one year with MRI and PET - CECT demonstrated continued regression of treated brain metastasis and further increase in necrosis of kidney tumour without any new metastasis.
At her last follow-up, the patient had good performance status (ECOG 0), no headache, bone pain or any urinary symptoms.
Discussion
Historically, RCC has been considered resistant to standard fractionation of radiation. This resistance can be overcome by the ablative dose of radiation leading to endothelial damage, stromal breakdown, intramitotic death and activation of ceramide pathways.
The first report of SBRT targeting primary RCC was published in 2003. Subsequently, there has been an increase in utilisation of SBRT for primary RCC with excellent local control. There are numerous publications on the effectiveness of SBRT in post nephrectomy oligometastatic setting. The pattern of response post SBRT is seen in the form of decrease in enhancement, increase in necrosis, and slow, but, gradual decline in the size of the lesion. Many fast-growing tumours shrink very rapidly with SBRT, but renal tumour shrinks gradually. More importantly, there is development of necrosis within the tumour and sometime loss of enhancement on CT scan/MRI can be seen. It has also been used to delay or defer systemic therapy in low and intermediate IMDC risk groups.
We have applied the concept of total ablative therapy, i.e. SBRT to both primary tumour and oligometastatic sites followed by systemic therapy when suitable. Patients were given synchronous delivery of SBRT to oligometastatic site, including primary tumour, within five days. Majority of kidney SBRT series have reported very low rates of toxicity. The International Radiosurgery Oncology Consortium for Kidney (IROCK) published a meta-analysis in 2022. It reported an impressive local control with manageable toxic effects.
It demonstrated a local control rate of 98% for all tumours with overall survival of 70% and cancer- specific survival of 92% when treating kidney tumours. In the recently published individual patient data meta-analysis, a five-year local control rate of 95% was reported. Studies from Japan reported five-year local (kidney) control of 94%. Although the follow-up duration of our patient was short (12 months), we reported complete control both in the brain and the kidney.
The current case emphasises the role of Total Ablative Radiosurgery/SBRT in oligometastatic cohort with intact kidney cancer, but in medically unfit patients or those who refuse surgery.
Dr. Shyam Singh Bisht
Associate Director - Radiation Oncology
Cancer Institute
Medanta - Gurugram
Dr. Tejinder Kataria
Chairperson - Radiation Oncology
Cancer Institute
Medanta - Gurugram
Medanta@Work
Reverse Takotsubo Cardiomyopathy: A Rare Diagnosis
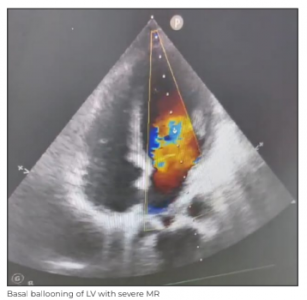
Takotsubo cardiomyopathy, also known as apical ballooning syndrome or stress cardiomyopathy, occurs when an emotionally or physically stressful event causes the heart’s left ventricle to dilate, leading to acute heart failure. The condition was first described in 1990 in Japan with the name being derived from a centuries-old octopus trap used in the country. In patients with Takotsubo cardiomyopathy, apical ballooning of the left ventricle gives the heart an appearance similar to the shape of pots as seen on a cardiac ventriculogram.
Its signs and symptoms are similar to acute mayocardial infarction (MI) with similar electrocardiogram (ECG) and biomarker indications. So, it often goes undiagnosed until a coronary angiography is performed and reveals no blockage. What makes our case rare is that the patient presented with reverse Takotsubu cardiomyopathy wherein there is left ventricular (LV) basal hypokinesis/akinesis. It typically presents with chest pain, and dyspnoea after a stressful event with complications, such as pleural effusion, pericardial effusion, and LV thrombus.
Case Study
A 36-year-old female presented in the Emergency (ER) of Medanta - Patna on inotropic support and non-rebreather (NRB) mask with shortness of breath. She had reportedly sustained a fall from the second floor of her house, and was treated conservatively at another hospital over the last two days. Her documented injuries included an injury to the left hip and chin with no loss of consciousness, ENT bleed, seizure or vomiting.
Her recorded vital statistics were: blood pressure (BP) of 90/60mmHg (started on noradrenaline), respiratory rate of 15-20 breaths/ min and saturation of 97-99% in room air.The initial investigations, which included echocardiography (Echo), revealed left ventricular ejection fraction (LVEF) of 70%. Her troponin test was negative, computed tomography (CT) of the pelvis showed a fractured pelvis for which traction was applied while CT brain and arterial blood gas (ABG) test were normal.
On Day 2, post trauma, her oxygen requirement increased with further decrease in BP. Repeat troponin test was positive and repeat Echo revealed LVEF of 27%. In view of her deteriorating condition, she was referred to Medanta - Patna on Day 3 of her injury.
The patient was brought to the Medanta - Patna ER on ionotropic (noradrenaline) and oxygen support. Extended focused assessment with sonography in trauma (eFAST) was negative, ABG revealed acidosis with lactate of 8.59, Echo was suggestive of LV basal hypokinesia, EF of 20%, moderately severe mitral regurgitation (MR), Grade-3 diastolic dysfunction and dilated inferior vena cava (IVC).
Following intubation in the ER, the patient was immediately shifted to the intensive care unit (ICU) under the Critical Care Team. During the course of her admission, the patient underwent high-resolution computed tomography (HRCT) of the thorax, serial chest X-ray, haematological and biochemical tests, including quantitative troponin I and coronary angiogram. The significant findings were: troponin I (quantitative) of 8788ng/L; D-dimer 1947ng/ml; procalcitonin 3.2ng/ml; HRCT chest showed bilateral ground glass opacities while coronary angiogram study, done on Day 7 of injury, was normal.
After being transferred to the ICU, the patient was continued on noradrenaline and dobutamine support along with injections atracurium, fentanyl, KCl, diuretics, and intravenous antibiotics. Respiratory support was maintained on pressure regulated volume control (PRVC) mode of ventilation with 100% fraction of inspired oxygen (FiO2) in prone position based on ABG.
Overnight improvement was seen in saturation with decreased FiO2 requirement, decreased inotropic support and improvement in ABG with settled acidosis and decreased lactate. The patient was extubated after 48 hours of admission following continuous positive airway pressure (CPAP) trial and kept on non-invasive ventilation. On Day 4 of admission, the patient achieved stable vitals without ionotropic support and her blood oxygen saturation was maintained with room air. She was discharged on Day 5 of admission. Reverse Takotsubu Syndrome is a diagnosis of exclusion. A correct diagnosis with proper systemic supportive care is beneficial for the patient. It is necessary that the treating clinician should have the diagnosis in the back of their mind while dealing with such cases of trauma.
Dr. Neha Singh
Associate Consultant - Institute of Critical
Care and Anaesthesiology
Medanta - Patna
Dr. Prabhat Kumar
Senior Consultant - Critical Care
Institute of Critical Care and Anaesthesiology
Medanta - Patna
Dr. Kishore Jhunjhunwala
Director - Critical Care Medicine
Institute of Critical Care and Anaesthesiology
Medanta - Patna
Mighty Mites: An Interesting Case of Pigmented Demodicidosis
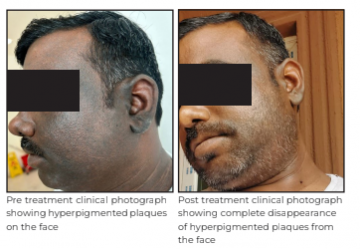
A 30-year-old male presented to Medanta - Lucknow with hyperpigmentation on skin and thick plaques over his entire face extending beyond the ears; no involvement was noticed elsewhere on the trunk and the body. The condition had developed over the last one year. Clinical differential diagnoses were lichen planus pigmentosus and Riehl's melanosis. There was no history of sun exposure, local application of any topical steroid or cosmetic products.
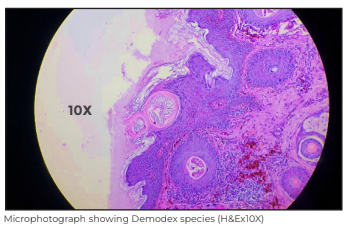
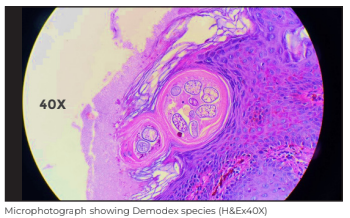
Skin biopsy showed follicular dilatation with multiple mites of Demodex species in the follicular infundibulum, dense homogenous eosinophilic material around the mites, perifollicular inflammation and sebaceous gland hyperplasia. A final diagnosis of Pigmented Demodicidosis was rendered - a diagnostic surprise to both the clinician and the histopathologist.
The patient was treated with 1% topical Ivermectin cream, to be applied on skin at bed time for six months, and oral tablet Ivermectin 12mg, once weekly for three weeks, along with capsule Isoretinoin 20mg, once daily for six months. The patient responded well and the plaques disappeared completely within six months.
Discussion
Pigmented Demodecidosis is an under-recognised entity and is not included as a cause of facial hyperpigmentation. Literature is scant regarding facial hyperpigmentation casued by Demodicidosis.
Demodex mites are minute arthropods that are normal inhabitant ectoparasites of the pilosebaceous units of the skin as a part of the normal skin flora. There are 65 species of Demodex and only two are found on the human body - Demodex follicularis, in hair follicles, and Demodex brevis, deep within the sebaceous glands. Demodex follicularis are larger of the two and often seen in aggregates, whereas Demodex brevis are usually solitary and produce infections in the eye (acute blepharitis and keratoconjunctivitis), rosacea and subclinical folliculitis on the face.
Demodicidosis is common in India, mostly asymptomatic and remains undiagnosed until there is a cosmetic concern or unusual presentation like in our case. Tissue biopsy or dermoscopy needs to be done for a correct diagnosis. Dermatologists and pathologists need to be aware of facial hyperpigmentation as a cause of Demodex-related infection otherwise the diagnosis may be missed. Patients can be treated with anti-demodectic medication and the prognosis is excellent.
For this under-recognised association with facial pigmentation, the term “pigmented demodicidosis” has been proposed recently to be added to the list of causes of facial hyperpigmentation.
Dr. Madhu Mati Goel
Director - Department of Pathology and
Laboratory Medicine
Medanta - Lucknow
Dr. Niti Singhal
Senior Consultant - Cytopathology
Department of Pathology and Laboratory
Medicine
Medanta - Lucknow
Dr. Shefali Porwal
Consultant - Dermatology
Medanta - Lucknow
Spotlight
Medanta Launches World's First Heart Tunnel to Strengthen Awareness on Heart Health
In commemoration of World Heart Day, and to strengthen the fight against heart disease, Medanta Hospitals at Gurugram, Lucknow and Patna installed the ‘World's First Heart Tunnel’. A 3D structure - 12 feet in height, 8 feet in width, and an impressive 20 feet in length - the tunnel was an educational exhibit that provided insight into the structure of the heart, how it functions, and what it sounds like. Through LED screens installed in the tunnel, patrons gained insight on the various types of cardiac procedures (interventional and surgical), devices used to address heart ailments as well as learnt about heart-healthy practices and those that are detrimental. Offering an immersive and visually stimulating experience - the tunnel was a unique medium through which medically relevant information was disseminated, allowing for a high recall value. The hospitals organised several community awareness programmes, symbolising Medanta's dedication to combating cardiac diseases.

Welcome Onboard

Dr. Ashish Kumar Jha
Director - Gastroenterology
Medanta - Patna
Gastroenterologist with expertise in advanced diagnostic and therapeutic endoscopy, both adult and paediatric. He specialises in endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), enteroscopy, EUS-guided pancreatico-biliary procedures, endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD).
 Dr. Raghav Shrotriya
Dr. Raghav Shrotriya
Senior Consultant - Plastic, Aesthetic and Reconstructive Surgery
Medanta - Gurugram
Plastic surgeon with expertise in hand surgeries, brachial plexus surgery and reconstructive microsurgery. He also specialises in facial surgeries, including rhinoplasty, cleft surgeries and maxillofacial trauma.
 Dr. Mayank Chugh
Dr. Mayank Chugh
Consultant - Internal Medicine
Medanta - Gurugram
Physician with expertise in diagnosis and management of infections across various specialities. He specialises in the treatment of gastroenterology and liver diseases.
 Dr. Abhishek Kumar
Dr. Abhishek Kumar
Consultant - Neurology
Medanta - Patna
Neurologist with expertise in managing neurological disorders. He specialises in the treatment of epilepsy, headache, cognitive impairment, stroke, neuro muscular and movement disorders.
 Dr. Alka Adlakha
Dr. Alka Adlakha
Consultant - Clinical and Preventive Cardiology
Medanta - Gurugram
Cardiologist with expertise in clinical and preventive cardiology, critical cardiology in addition to treadmill test, 2D echocardiogram, stress and dobutamine stress echocardiogram. She also specialises in the treatment of heart failure.
 Dr. Avishek Chatterjee
Dr. Avishek Chatterjee
Consultant and Head - Department of Emergency and Trauma Care
Medanta - Ranchi
Critical care clinician with expertise in managing cardiac emergencies, neurological emergencies, chest emergencies and gastrointestinal emergencies.
 Dr. Santosh Kumar
Dr. Santosh Kumar
Consultant - Paediatric Haemato Oncology and BMT Physician
Medanta - Patna
Medical and haemato oncologist with expertise in paediatric haematology and oncology. He specialises in bone marrow transplant, immunotherapy, cellular therapy and in the treatment of benign haematological disorders, including thalassaemia, sickle cell disease, all kinds of haematological cancers, including leukaemias, lymphomas, and solid tumours, including hepatoblastoma, Wilm’s tumour, brain tumours, in addition to treating primary immunodeficiency disorders.
 Dr. Tushar Bharat Patil
Dr. Tushar Bharat Patil
Associate Consultant - Aesthetic, Plastic and Reconstructive Surgery
Medanta - Gurugram
Plastic surgeon with expertise in reconstructive surgery after trauma and cancer in addition to hand and cosmetic surgery.
 Dr. Arun Prasad
Dr. Arun Prasad
Associate Consultant - Paediatric Gastroenterology and Hepatology
Medanta - Gurugram
Paediatric gastroenterologist with expertise in paediatric and adolescent gastroenterology and hepatology. He specialises in endoscopy, and in the treatment of liver diseases, pancreatitis, irritable bowel syndrome in addition to nutritional issues in children and adolescents.
 Dr. Vijay Kumar Singh
Dr. Vijay Kumar Singh
Associate Consultant - Nephrology and Kidney Transplant Medicine
Medanta - Ranchi
Nephrologist with expertise in managing complex kidney diseases, haemodialysis and peritoneal dialysis,interventional nephrology in addition to kidney transplantation.






