THE EXCHANGE | Newsletter - May 2023
Multisystem Inflammatory Syndrome in Children Returns with Surge in COVID-19 Infections
Multisystem inflammatory syndrome in children (MIS-C) is a rare but serious complication associated with COVID-19. The Centre for Disease Control (CDC) re-defined MIS-C in January 2023 as a fever in any person under 21 years of age with new onset/organ manifestations in more than two categories, such as cardiac, shock, gastrointestinal, mucocutaneous, and haematological, with high C-reactive protein (CRP30mg/L) meeting with lab criteria of COVID-19 infection, i.e. detection of SARS-CoV-2 RNA/ SARS-CoV-2 specific antigen or antibodies. In the last two months, we have seen an increase in cases of novel coronavirus across India. With each resurgence of COVID-19, there is an increased risk of MIS-C cases as well. We report one such case that presented with shock and acral gangrene.
Case Study
A 10-month-old boy presented with fever for 8 days, diarrhoea and vomiting for 4 days, and rash and swelling all over the body for 2 days. He was being treated for sepsis at another centre and then referred to Medanta - Gurugram with worsening shock and encephalopathy. At the time of admission, he was encephalopathic, had poor perfusion and on vasopressor support by peripheral vein. He had bluish discoloration of peripheries (lower and upper limbs) with necrotic patch over legs and tip of the nose.
He was intubated in view of worsening shock and sensorium. Shock was managed with vasopressors along with other supportive and neuroprotective measures. Initial investigations showed anaemia (Hb 6.5gm/dL), lymphopenia (absolute lymphocyte count 900) and severe thrombocytopenia (platelet count 12000/cumm). Inflammatory markers were also found to be elevated (CRP 260 mg/L, Ferritin 1500ng/ml) and there was coagulopathy with very high D-dimer levels (>10000). Provisional diagnosis of septic shock with disseminated intravascular coagulopathy (DIC) with encephalopathy (meningococcaemia) was considered and child was started on broad spectrum antibiotic with acyclovir.

For the next 48 hours, the child responded suboptimally to initial antibiotics and supportive care. He had persistent fever, haemodynamic instability and worsening acral gangrene with high inflammatory markers. As the blood, cerebrospinal fluid (CSF) culture and COVID-19 RT-PCR reports were negative, MIS-C was suspected. COVID-19 antibodies were sent for examination, which came out to be positive with a reading of >250 against the usual cut-off of <50. He was subsequently treated with immunoglobulin (IVIG) at 2gm/kg over the next 24 hours and steroids at 2mg/kg/day following which there was rapid defervescence and resolution of shock. Further progression of the gangrenous zone and associated proximal edema also reduced. Inflammatory markers also improved along with D-dimer levels.
He was extubated after 6 days of ventilation. Subsequent course of physical and nutritional rehabilitation was uneventful. He was discharged after 2 weeks of in-patient stay on oral nutritional supplements. The patient is doing well on regular follow-up.
Discussion
This case highlights atypical cutaneous manifestation (digital gangrene) of MIS-C along with more typical features such as shock and hyperinflammatory state. Common cutaneous manifestations of MIS-C include Kawasaki disease-like polymorphic maculopapular or diffuse erythrodermic rash. Acral gangrene reflects severe distal hypoperfusion as it is a relatively infrequently reported finding in MIS-C. Proposed mechanisms of this phenomenon include endothelial dysfunction and micro-embolic formation. Contributory risk factors may include the use of vasopressors and cardiac dysfunction. Clinicians must be aware of this presentation of MIS-C as increased case load is anticipated in the coming months. Prompt recognition and early use of immunomodulatory therapy results in suppression of the cytokine storm and restoration of normal microcirculation with positive outcome.
Dr. Rajiv Uttam
Director and HOD - Paediatrics, PICU
and Paediatric Emergency
Institute of Women and Children
Medanta – Gurugram
Dr. Praveen Khilnani
Chairman - Paediatrics, Paediatric
Pulmonology and Paediatric Critical care
Institute of Women and Children
Medanta – Gurugram
Dr. Mukul Pandey
Consultant - Paediatrics, PICU
and Paediatric Emergency
Institute of Women and Children
Medanta – Gurugram
Medanta@Work
Journey of Becoming Seizure-free after 25 Years of Epileptic Episodes
Epilepsy affects about 1% of the population in India and it is one of the leading causes of disability resulting from a neurological condition. Around 40% of these patients are very likely to have uncontrolled epilepsy i.e. Drug-Resistant Epilepsy (DRE) causing persistent seizures that continue despite adequate trial of two or more anti-seizure medications (ASMs).
Case Study
We present the case of a 25-year-old male from Nepal with a history of normal birth and developmental milestone attainment. He started having recurrent seizures when he was one year of age. His medical history showed that he would get seizures every day and on many days he would get up to 10-12 seizure attacks each lasting 2-3 minutes. Over the years, he consulted multiple physicians, neurosurgeons and neuro-physicians and was prescribed multiple antiepileptic drugs without any significant relief. He presented to Medanta - Gurugram for treatment where his case was assessed in detail.
During his seizures, the patient would initially have palpitations and uneasiness following which he would run about here and there, and hug his parents in fear. He would then have a staring look with unresponsiveness and some vague movements such as chewing, lip smacking or rubbing his hands.
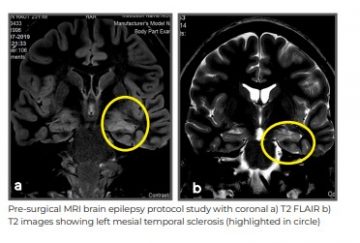
Based upon his history alone, a diagnosis of mesial temporal sclerosis was made. Considering drug resistance, advanced treatment options, including epilepsy surgery, were discussed. The patient was admitted for pre-surgery evaluation. Long-term video electroencephalogram (EEG) monitoring was done. During the hospital stay, he had multiple seizures, which were recorded by the advanced video EEG machine showing clear origin from left temporal area. As there was a clear focus over the left mesial temporal region for origin of patient’s seizures - confirmed by video EEG and the MRI brain - he was identified as an ideal candidate for epilepsy surgery. The patient underwent left anterior temporal lobectomy with amygdalo-hippocampectomy with intra-operative electrocorticography (ECOG).
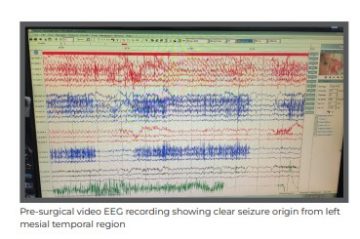
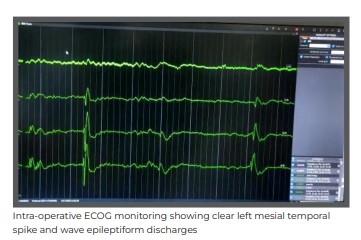
ECOG is an advanced monitoring of the electrical activity of the brain. It is available in very limited tertiary care centres in India and is done intra-operatively to tailor the surgery margins of the resection. With the patient being right-handed and clear dominance of left hemisphere on his neuro-psychometric evaluation, his language areas were in the left hemisphere of the brain, including areas of comprehension and speech. During anterior temporal lobectomy with amygdalo-hippocampectomy, careful considerations were made by the surgeon to protect these areas during resection.
The removed area was sent for histopathological analysis and it was suggestive of mesial temporal sclerosis with focal cortical dysplasia. The surgery was successful, and the patient has remained completely seizure free post operatively. From suffering multiple seizures every day to becoming seizure-free, the patient’s quality of life has drastically improved.
Discussion
Mesial temporal sclerosis is the most common form of focal epilepsy with drug resistance which can be treated by surgery. The temporal lobes are the most common brain region to develop epileptogenicity. In the 20th century, the term ‘psychomotor epilepsy’ was introduced by Gibbs and Gibbs to describe the characteristic psychic and emotional semiological findings in seizures originating from mesial temporal area. This seizure type is often misdiagnosed and patients are treated as psychiatric patients because of lack of awareness about these seizures as they are quite different from the commonly encountered grand mal and petit mal seizures. This is especially common in developing countries such as India and Nepal. These patients commonly have DRE. In patients who have DRE, surgery remains the treatment of choice if a surgically amenable lesion can be found.
Epilepsy surgery is of various kinds, including lesionectomy, hemispherotomy, corpus callosotomy, deep brain stimulation (DBS), vagal nerve stimulation (VNS), responsive neurostimulation (RNS) etc.
At Medanta-Gurugram, these are performed regularly with excellent post-surgical seizure-free outcomes.
Dr. Arun Garg
Director
Institute of Neurosciences
Medanta – Gurugram
Dr. Sudhir Dubey
Chairman - Endoscopic Portal Minimal
Invasive Neurosurgery
Institute of Neurosciences
Medanta - Gurugram
Dr. Atma Ram Bansal
Associate Director - Epilepsy Programme
Institute of Neurosciences
Medanta – Gurugram
Pre-op Planning Key for Abdominal Wall Reconstruction
Incisional hernia is a problem commonly seen after any abdominal surgery. Studies estimate that up to 20% of open abdomen surgeries may result in formation of incisional hernia requiring further surgery. Large ventral abdominal wall hernias can significantly impair the quality of life, and their repair has been associated with a high rate of complication and recurrence. To lower these risks, several techniques have been implemented, such as anterior and subsequently posterior component separation with transverse abdominis muscle release (TAR).
A hernia left untreated usually enlarges with time, sometimes resulting in formation of massive hernia sacs with over 20%-25% of the intra-abdominal visceral contents residing in the hernia sac, known as loss of domain (LOD). Large ventral hernias with LOD are often a challenging problem to fix. A technique, known as Peritoneal Flap technique, popularised by a group of surgeons from Edinburg, utilises the hernia sac as a flap to reduce the tension on the hernia closure, with reinforcement by a prosthetic mesh. Massive ventral hernias with LOD require extensive planning and sometimes pre-operative optimisation with injection of botulinum toxin (Botox) to enhance chances of a successful surgery and minimise complications. A Botox injection in the lateral abdominal wall has also been shown to induce a temporary chemical paralysis of the abdominal wall muscles, lasting a few months thus facilitating the hernia surgery. This needs to be done at least four weeks before the planned surgery. We present the case of a patient with a large incisional hernia with loss of abdominal domain.
Case Study
A 48-year-old female patient with co-morbidities, including Type-2 diabetes and hypertension, presented to Medanta - Gurugram with a large recurrent incisional hernia. After having undergone a hysterectomy, she developed an incisional hernia which was followed by an Onlay Mesh Repair but with recurrence soon after. Due to recurrence after her first operation, she became very fearful of surgeries and refused intervention till her hernia became very large in size with ulceration of the overlying skin leading to a very poor quality of life. The large hernia with loss of abdominal domain impacted her day-to-day functioning, and limited her mobility with progressive weight gain.
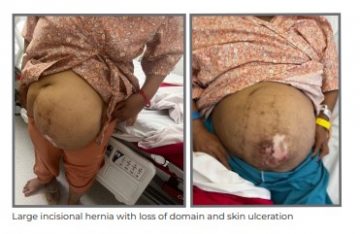
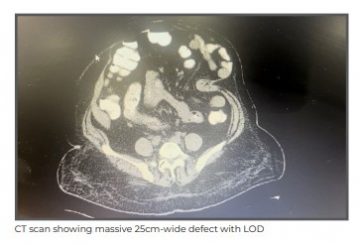
She was evaluated with the help of a CT scan that showed a large 17x25 cm midline incisional hernia with almost 50% contents of the abdominal cavity in the hernia sac. Given the massive nature of the hernia, she was optimised for surgery with Botox infiltration in the abdominal wall muscles. A total of 200 units of Botox was infiltrated at different sites in all three lateral abdominal wall muscles. After six weeks, she was revaluated with a CT scan that confirmed laxity of the muscles with 4-5 cm reduction in size of the hernia defect, after which definitive surgery was performed.
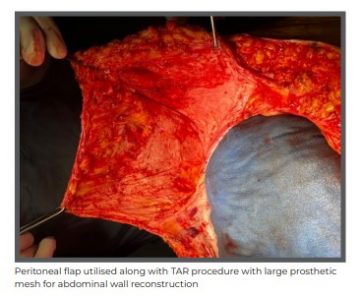
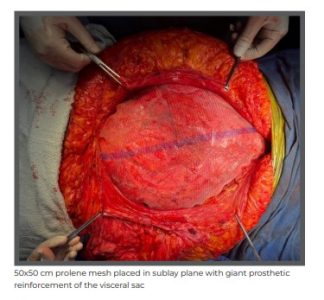
She underwent a posterior component separation surgery with TAR combined with the use of peritoneal flap hernioplasty. A large 50x50 cm polypropylene mesh was placed in the sublay plane. The peritoneal flap was divided in midline and left attached to posterior sheath on one side and anterior sheath on the other side, enabling a tension-free closure despite the massive nature of the defect. The previous scar was excised and abdominoplasty was also done.

The surgery lasted for 6 hours and the patient could be extubated immediately after the procedure without signs of Abdominal Compartment Syndrome. She did not require ICU stay and could be monitored in the ward. She was discharged on Day 7 of the surgery and sutures were removed on outpatient basis on post- operative Day 14. Two months after the surgery, the patient was doing well with improved quality of life.
Dr. Vikas Singhal
Senior Consultant - GI Surgery, GI Oncology
and Bariatric Surgery
Institute of Digestive and Hepatobiliary Sciences
Medanta – Gurugram
TechByte
World's Fastest CT Scanner Now at Medanta
Medanta - Gurugram has installed SOMATOM Force - the world’s fastest CT scanner with a scanning speed of 737 mm per second (2 x 192 Slices Dual Source CT scan).
The advanced AI based scanner is equipped with two CT tubes and two detector systems, each capable of acquiring 192 slices combining the power and precision of two CT Scanners in one for unmatched image quality.
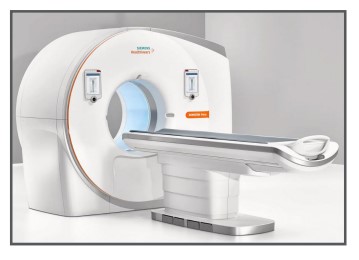
Key Highlights:
- Precision 4D scanning: Helps in high-precision diagnosis, reliable therapy response evaluation, and improved patient care.
- Walk-in-walk-out coronary scanning: Cardiac CT angiogram can be performed for any patient with any heart rate without any beta blocker.
- Best-in-class AI technology: High power, speed, and automated dose management help precisely adapt scanning parameters for any patient. The automated fast integrated workflow supports reproducible image quality.
- Ultra low-dose scanning: The machine’s unique tin filter technology shields patients from clinically irrelevant low-energy radiation. With this, excellent results can be delivered at dose levels comparable to conventional X-rays. This also facilitates early detection of cancer.
- Free-breathing CT scan: The powerful technology allows scans without any compromise in image quality up to the next level with precise details. Chest and abdomen scanning can be performed without breath- old in less than a second.
- Kidney-friendly scanning: Allows to routinely perform exams at 70-90 kV, even with adults. This reduces the quantity of contrast media required and lesser complications for patients with renal insufficiencies.
- Sedation-free, low-contrast, free-breathing paediatric CT: Scanning the most challenging paediatric patients with extremely high heart rates is possible within a fraction of a second for congenital pathologies or other diseases.
- Precise and dose-neutral Dual Energy (DE): Dual Energy CT can add tissue and material information to morphology, enabling a better treatment regime and follow-up.
- Whole-body advanced CT procedures: Performing these procedures becomes routine for neuro imaging, cardio vascular imaging, paediatric imaging, oncology imaging, traumatology imaging, urology imaging, orthopaedic imaging, etc. due to AI based automation.
- Well-suited for obese patients: With exceptional image quality at lower kV, even obese patients can be scanned.
Spotlight
Medanta Conclave 2023 held in Patna
Jay Prabha Medanta Super Specialty Hospital organised 'Medanta Conclave 2023: Recent Advances in Medical Science', a two-day multispecialty CME on I5th and 16th April 2023.
Hon’ble Chief Minister of Bihar Shri. Nitish Kumar Ji inaugurated the event in the presence of
Dr. Naresh Trehan (Chairman and Managing Director, Medanta) and Mr. Pankaj Sahni (Group CEO and Director) in Patna.

The conclave - organised under the leadership of Medanta’s Dr. Ajay Kumar Sinha,
Dr. Rajiv Ranjan Prasad and Dr. Kishore Jhunjhunwala - was aimed at improving awareness among doctors on recent advancements in the fields of cardiac science, neuroscience, kidney disease, lung disease, cancer, orthopaedics, organ transplantation, and minimally invasive and robotic surgery.
With over 500 distinguished doctors from Bihar in attendance, the panel discussions led by Medanta’s super-specialists - including Dr. Randeep Guleria, Dr. Rajiva Gupta, Dr. Prasun Ghosh, Dr. Deepak Sarin, Dr. Pramod Kumar, Dr. Sanjay Kumar, Dr. Sanjoy Kumar, Dr. Mukund Prasad and Dr. Prabhat Ranjan – were an effort towards building a more robust health care system in the state. Dr. Naresh Trehan and Mr. Pankaj Sahni also felicitated the state’s top doctors for their outstanding and lifelong contribution to the field of medicine.
Kudos

Congratulations Dr. Aditya Aggarwal (Vice Chairman - Plastic, Aesthetic and Reconstructive Surgery, Medanta, Gurugram) on being elected as the President of the Indian Association of Aesthetic Plastic Surgeons (IAAPS) - the only organisation representative of country’s qualified Plastic Surgeons practicing aesthetic plastic surgery. An accomplished plastic surgeon, Dr. Aggarwal specialises in aesthestic surgeries, reconstruction surgeries for breast, and head & neck cancer patients, and facial reanimation surgery for facial deformities.
Welcome Onboard
Dr. Kunjahari Medhi
Senior Director - Medical Oncology and Haemato-Oncology
Medanta - Gurugram
Medical oncologist with over 25 years of experience and expertise in all types of chemotherapies, targeted therapy, immunotherapy and all other modern forms of systemic cancer treatments, including stem cell or bone marrow transplants, and management of oncological emergencies
Dr. Amanjee Bharti
Consultant - GI Surgery, GI Oncology and Bariatric Surgery
Medanta - Patna
Gastrointestinal surgeon with expertise in advanced laparoscopic surgery. He specialises in hernia surgery, hepatobiliary surgery and proctology surgery in addition to laparoscopic and open gastrointestinal emergency surgeries.






