THE EXCHANGE | Newsletter May 2020
Managing COVID-19 Cases
COVID-19 is an emerging, rapidly evolving situation.
The treatment guideline for the disease is also evolving. As per the current ICMR guideline, while managing COVID-19 patients, the first and the most important step is to differentiate between a symptomatic and an asymptomatic patient. This can be easily accomplished by taking detailed history. The next step is to categorize the patient as a suspected or a non-suspected case of COVID-19. This is done with the help of exposure risk stratification assessment as prescribed by the ICMR.
Identification and Stratification of Symptomatic Patients
- A patient exhibiting mild symptoms including low-grade fever, mild cough, throat irritation without hemoptysis or breathlessness is classified as a mild case.
- A moderately symptomatic patient experiences above symptoms in moderation. The person has respiratory rate between 15 and 30 per minute, and has signs of respiratory distress like flaring of nostrils and use of external muscles like those of neck. Indrawing of the chest and SpO2 between 90 and 94% are also signs of a symptomatic patient.
-
A severely symptomatic patient has high respiratory distress with respiratory rate of over 30 per minute. The patient struggles to even speak a sentence. Pulse oximetry is typically less than 90% and the patient is unable to do activities of daily life.
Who is a suspected case?
As per the ICMR guideline, suspected category of patients include:
- Individuals with a history of international travel in the preceding two weeks exhibiting symptoms
- Symptomatic healthcare providers, whether in hospital or diagnostic lab engaged directly / indirectly with COVID-19 patients exhibiting upper and lower respiratory tract infection
-
All hospitalized patients with severe acute respiratory infection, pneumonia, breathlessness, hemoptysis, respiratory distress requiring oxygen
- Close contacts of a confirmed COVID-19 patient and healthcare workers who have examined this patient.
What is contact?
Without PPE contact (distance<1 metre) of more than 15 minutes with a suspected or confirmed case two days prior to the onset of the symptoms and up to 14 days afterwards is considered significant contact.
Depending upon symptoms and suspicion, there are four possible patient categories:
-
Asymptomatic Non-suspects
-
Asymptomatic Suspects
- Symptomatic Suspects
-
Symptomatic Non-suspects
Management of Asymptomatic Non-suspects
-
Situation assessment to understand why the individual sought consult
- Awareness about precautionary measures and disease transmission
- Anxiety counselling if required
Management of Asymptomatic Suspects
-
Awareness about precautionary measures, disease transmission and minimizing risk of spread
-
Strict use of mask and hand hygiene
- Immediate medical attention in case of symptoms such as fever, cough and sore throat
-
COVID-19 test
- Confinement / Isolation at home
Management of Symptomatic Suspects
- Categorization into mild, moderate and severe as explained earlier
- Inform the concerned health authorities
- Strict isolation from family until hospitalization

- Adherence to social distancing, hand hygiene, separate bedroom, bathroom
- Advise Paracetamol for fever after noting previous medical history and drug allergies
Management of Mildly Symptomatic Suspects
- Admission to a COVID Care Center where symptomatic treatment is provided and COVID test is done
- Monitoring by healthcare providers in line with prescribed protocol. Routine investigations are done
- If COVID test is positive, the patient is moved to a separate facility where confirmed cases are admitted
-
If COVID test is negative, the individual is discharged and advised general preventive precautions
Management of Moderately Symptomatic Suspects
- Admission to a COVID Care Center where symptomatic treatment is provided and COVID test is done
- If COVID test is positive, the patient is moved to a COVID facility where confirmed cases are admitted. Patient is monitored for severity and disease progression and treated as per protocol
- If COVID test is negative, the patient is shifted to non-COVID facility and investigated / treated for any alternate underlying conditions
Management of Severely Symptomatic Suspects
- Immediate admission to the closest, dedicated COVID centre
- If the test is positive, the patient is shifted to a confirmed COVID ICU and is managed in line with the protocol
- If the test is negative, the patient is admitted to non COVID area and investigated further while following all infection control practices
Management of Symptomatic Non-suspects
-
Categorization into mild, moderate and severe as explained earlier
- Mild cases should stay at home, seek teleconsult, and test for COVID if symptoms aggravate
- Moderate cases should be admitted to hospital, assessed for the cause of symptom and treated accordingly
- Severe cases should be admitted to the ICU. If they have respiratory issues, they should be treated like a suspected case. In case of any other symptom such as chest pain, symptomatic management is advised
As mentioned earlier, COVID-19 infection is a dynamic situation and ICMR guidelines are changing time-to-time. It’s advisable to stay updated and informed.

Tele-health in the Times of COVID-19
At a time, when social distancing is among the major measures used to fight COVID-19 pandemic, telemedicine is stepping-up as a key technology for safe and efficient communications.
The World Health Organization mentioned telemedicine among essential services in “Strengthening the Health Systems Response to COVID-19” policy. According to a new WHO policy, telemedicine should be one of the alternative models for clinical services and clinical decision support.
The Center for Disease Control and Prevention in the US and the National Health Service in the UK have recommended the use of telemedicine for identifying high-risk patients and treating other illnesses during the outbreak.
More recently, the Union Health Ministry of India also approved the use of telemedicine by registered medical practitioners to treat COVID-19 patients remotely or by using telemedicine tools.
Imbalance and shortage of healthcare professionals, together with unequal quality and access to healthcare services are challenges telemedicine can offer a solution to.
Other benefits telemedicine offers include:
- Elimination of risk of disease transmission
- Saved time and commute
- Increased volume of consults an individual practitioner can attend to
- Opportunity to expand one’s reach to remote locations
- Reduced cancellations and no-shows
-
Eliminated waiting time leading to better patient satisfaction
- Conservation of protective gear for healthcare workers
At Medanta, all our super-specialty doctors are available for tele-consults 24X7.
Our Internal Medicine team is engaged in virtually advising and counselling people on COVID-19, and directing them to the government approved centres.
Telemedicine@Medanta
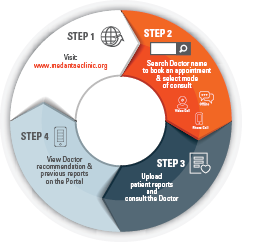
To book a tele-consult
Visit www.medantaeclinic.org
or
Download Medanta - eCLINIC mobile app

or
Call +91 124 4141 414
Patient Safety in Times of COVID
Amidst the COVID outbreak, as a tertiary care hospital, Medanta stays committed to delivering healthcare seamlessly while staying focused on safety of our patients, attendants and staff. Stringent infection control protocols have been instituted to ensure safety of non-COVID patients as we treat them seamlessly.
Safety @ OPD
- Screening of everyone entering the hospital is done with a thermal sensor. Patients and attendants are enquired about their history of fever, body ache, cold, cough or respiratory symptoms besides their history of travel in the last 15 days. If such history is detected, the visitor is directed to a dedicated Flu Clinic available in a separate, isolated area accessible from a different entry. Suspected cases are referred to government approved COVID treatment facilities.

- Only one attendant is allowed with a patient, and both are mandated to wear masks and sanitize their hands before they enter the facility. Visitors who don’t have a mask are provided a mask at the entrance.

- Q-managers are deployed to distance visitors from the reception staff.
-
Waiting lounges have been cleared off magazines, books and newspapers to prevent cross-usage. Separation of one metre is maintained between two individuals in the lounge.
- Door-knobs, handrails, cabinet handles, computer systems, floors and all other surfaces are cleaned every four hours with 1% solution of sodium hypochlorite (bleach). All access doors, that can be kept open are left open, to minimize human contact.
- Doctors are being encouraged to virtually consult patients using Medanta’s telemedicine app called Medanta e-Clinic. Extensive patient communication is being done to promote tele-consultation. Such virtual consults are available for anytime access of patient on the telemedicine app. The patient can also access all their health records including diagnostic results virtually.

- In chronic care situations such as cancer wherein patients require chemotherapy at a fixed interval of time, the executive staff has been trained to issue letters addressed to civic authorities, which allow patients to travel to the hospital during the lockdown situation.
-
Digital transaction is being encouraged.

Safety @ Emergency
When a patient reports to emergency, their history is taken while they are being triaged. The patient is enquired about travel history and any COVID symptoms such as fever, body ache, cold, cough or respiratory issues. In case there is slightest suspicion of COVID, the person is shifted to a separate zone where they are stabilized while following COVID infection control protocol and referred to a government approved COVID treatment facility. In absence of COVID suspicion, the patient is stabilized and transferred to an observation facility where treatment is initiated and sample is sent for COVID testing. Since Medanta has in-house COVID testing facility, it takes only 6-7 hours to get the results. Following a COVID negative report, the patient is shifted to ward as required. If ICU admission is required, the patient is admitted to a separate ICU designated for COVID result awaiting patients. After a negative report, the patient is shifted to the regular ICU.
Safety @ IPD
Any patient who requires hospital admission is first kept in the observation area where they are tested in-house for COVID. Only after a receiving a COVID negative report, which takes 6-7 hours, the patient is shifted to the ward. Until the COVID negative report comes, the patient is confined to the observation area, only allowed to use a lift dedicated to under-observation patients, and not allowed movement in the hospital except areas specifically designated for such patients.

If a patient comes for a planned surgery, they have the option of getting a COVID test done at Medanta or any other government approved facility. Test results are considered valid for a maximum of 48 hours.
Safety @ Observation Area
-
The observation area where COVID result awaiting patients are admitted is in a separate hospital wing with restricted access.
-
Dedicated staff manage this zone and they do not mingle with the rest of the hospital staff.
- Regular COVID screening is done for staff deputed in the observation area.
-
Infection control measures prescribed for COVID facilities are followed here.
-
The staff uses PPE as advised for COVID treating healthcare workers.
-
No attendants / visitors are allowed in this area.
Depending on the area the staff is deployed at, they wear appropriate PPEs and follow relevant infection control protocols.
All of the above measures ensure safety of our patients and staff so that healthcare, including consultation, surgery, day care procedures, gets delivered in an uninterrupted manner.
Is Your Clinic COVID Ready?
Healthcare workers are highly vulnerable to COVID-19 infection. Following measures can help you prepare your clinic and train your staff to safeguard against the highly contagious infection:
Before Patients Arrive
Prepare the clinic
- Classify routine and high-risk patients.
- Consider and plan for providing more telemedicine appointments.
-
Know how to contact government authorities if there is a positive case.
Prepare the waiting area and patient rooms
-
Provide supplies-tissues, alcohol-based hand rub, soap at sinks, masks and trash cans.
- Place chairs 3–6 feet apart, when possible. Use barriers (like screens), if possible.

- If your office has toys, reading materials, or other communal objects, remove them or clean them regularly.
-
Post signs at entrances and in waiting areas about prevention actions, cough etiquettes, social distancing, hand hygiene.
When Patients Arrive
-
Place staff at the entrance to ask patients about their symptoms.
- Provide symptomatic patients with tissues or facemasks to cover mouth and nose.
- Limit non-patient visitors. - Separate sick patients with symptoms.
- Allow patients to wait outside or in the car if they are medically able.
- Create separate spaces in waiting areas for sick and well patients.
- Place sick patients in a private room as quickly as possible. -
Use disposable sheet on the examination table and hand rub after each patient
- Fever and Respiratory Clinic should be run separately, preferably in the evening after regular OPD
After Patients are Assessed
-
After patients leave, clean frequently touched surfaces such as counters, beds and seating using approved disinfectants.
-
Provide at-home care instructions to patients with respiratory symptoms. Consider tele-health options for follow up.
- Encourage digital transactions.

Train and Prepare Your Staff
-
Ensure that clinical staff knows:
- The right ways to put on, use, and take off PPE safely.
- Recognize the symptoms of COVID-19 - fever, cough, shortness of breath.
- Implement procedures to quickly triage and separate sick patients. - Emphasize hand hygiene and cough etiquette for everyone.
- Ask staff to stay home if they are sick.
Source: Centers for Disease Control and Prevention
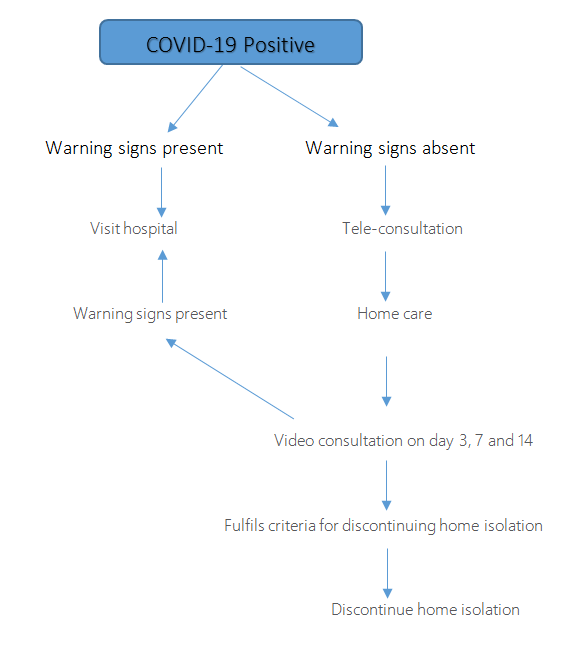
Home Triage Protocol for COVID Patients
Why is Home Care Required?
With increasing number of cases of COVID-19 admitting every patient in hospital will put serious pressure on our health care system. Since almost 80% patients have mild disease and may not require much medical intervention, most of these patients can be managed at home.
Who Can be in Home Care?
Patient and disease factors
- Patient is stable.
- Patient is willing to be in isolation.
-
Patient understands the disease process including warning signs.
Social factors
- Family members/caregivers are available at home, who understand the disease process.
-
A separate bedroom and toilet for the patient is available.
- Access to food and other necessities.
-
Access to gloves, face mask and other necessary medical supplies.
-
The patient and household members are capable of adhering to recommendations for home care.
Caregivers cannot include the following
- Age >65 years.
- Pregnant women.
- People who are immuno-compromised.
-
Those with chronic heart, lung, or kidney conditions.
Patient Care at Home
Stay at home
- Don’t panic
- Most people with COVID-19 have mild illness and are able to recover at home.
- Don’t leave home, except for medical care.
- Don’t visit public areas.
- Don’t use public transport.
Home isolation
- Stay in a separate room and use a separate bathroom.
- Take rest. Stay well hydrated.
- Wear face mask, maintain social distance.
-
For fever take tablet Paracetamol 650mg.
- For cough, get telephonic / video consult.
Cough etiquettes and use of mask
-
Cover your cough and sneezes with cloth or tissue paper.
-
Dispose the tissue or cloth carefully in a lid covered dust bin.
- Immediately wash hands with soap and water.
- Wear a cloth/ regular face mask if 3 layered mask is not available - over your nose and mouth at all times.
Hand hygiene
-
Wash hands with soap and water for at least 20 seconds or clean your hands with an alcohol-based hand sanitizer with at least 60% alcohol.
Avoid sharing personal household items
- Avoid sharing utensils, towels, and bedding.
-
After using these items, wash them thoroughly with soap and water.
House hold cleaning
Clean all surfaces that are touched often, like tabletops, and doorknobs in sick room and bathroom with disinfectant like 1% Sodium Hypochlorite.
For Care Providers at Home
Monitor the person for worsening symptoms.
-
Know emergency warning signs.
Prevent spread of germs when caring for the sick
-
Have the sick person stay in a separate room as much as possible.
- Have them use a separate bathroom.
- Flushing of toilet to be done after closing the lid of the commode.
- Avoid sharing personal household items, like utensils, towels, and bedding
- Have them wear a face mask when they are around people.
-
Wash your hands often with soap and water for at least 20 seconds after interacting with the sick person. If soap and water are not readily available, use a hand sanitizer that contains at least 60% alcohol.
- Avoid touching your eyes, nose, and mouth.
-
Wash clothes / bedding of the sick person thoroughly.
-If clothes / bedding is soiled, wear disposable gloves and keep the soiled items away from your body while washing. Wash your hands immediately after removing gloves.
-
Avoid having any visitors.
When to Report to Hospital/ Warning Signs*
-
Persistent Fever >1010F for 72 hours.
-
Breathlessness, feeling of air hunger, fast breathing rate.
- Blood in sputum (hemoptysis)
- Confusion, loss of consciousness, altered behaviour.
-
Severe abdominal pain with diarrhoea or vomiting
-
Pulse rate >110/min
- Systolic blood pressure (in mm hg)**} <100 ( If any 1 out of 8 is present)
- sPO2 on room air (in %)**}<94
* Medanta protocol
**Subject to availability of apparatus.
Access to Healthcare
- Patient should have access to health care professionals via video/tele consultation.
-
Patient should do video/tele consultation with their physician on 3rd, 7th and 14th day or earlier in case of warning signs
- Health care facility with emergency and ambulance service should be available in vicinity
-
Please notify the emergency, ambulance staff and physician about your COVID-19 status before planning to visit hospital.
When to Discontinue Home Isolation
- Patient no longer has a fever (without the use of medicine that reduces fevers) and,
- Other symptoms have improved (for example, cough or shortness of breath have improved) and,
-
Negative test at the end of 14 days of isolation.
-
If the test is still positive at 14 days, extend isolation to 21 days and repeat testing at the end of 21 days.
Home Triage Protocol
References
- https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html.
- https://covid-19.uwmedicine.org/Pages/default.aspx
Prepared by
Dr. Vikas Deswal, Dr. Sushila Kataria, Dr. A S Soin, Dr. Yatin Mehta






