THE EXCHANGE | Newsletter March 2022
Minimally Invasive Thoracic Aortic Aneurysm Repair by TEVAR
Thoracic aortic aneurysm refers to the condition in which there is an abnormal bulge in a weakened wall of the aorta in the chest area. Aortic dissections are classified into two types: Type B dissection involves a tear in the descending part of the aorta and may extend into the abdomen, whereas Type A dissection develops in the ascending part of the aorta just as it branches off the heart.
Thoracic endovascular aortic repair (TEVAR) is a minimally invasive procedure used to repair a thoracic aortic aneurysm or dissection. Indications for repair have typically been an aortic diameter size greater than 6 to 6.5 cm as the threshold where risk of repair is outweighed by the risk of rupture. Patients with aneurysms larger than 6 cm have a 14.1% annual risk of rupture, dissection, or death, compared with 6.5% for patients with aneurysms between 5 and 6 cm. Symptomatic aneurysms and aneurysms associated with a rapid growth rate of greater than 1 cm per year are considered to be at an increased risk for rupture and should be repaired.
Case Study
A 45-year-old male, known smoker and hypertensive, on treatment for hypertension since eight years presented with history of chest pain. He had been evaluated at another centre where a CT Aortogram was done which revealed a dissecting aneurysm of the thoracic aorta. He was referred to Medanta Lucknow. 2D Echo was done here which showed normal systolic left ventricular function with mild concentric left ventricular hypertrophy and grade 1 diastolic dysfunction. High normal aortic root size was noted. CT Aortogram was repeated which revealed dissecting aortic aneurysm involving descending thoracic aorta with thrombosed false lumen (10*7 cm) and focal dissection flap at D5-D6 level (18*9 mm) - residual flow channel in false lumen and Stanford Type B dissection. As the patient was symptomatic, repair was planned, and he was given both surgical and minimally invasive TEVAR option for management. He chose to undergo TEVAR under general anesthesia. After induction of anesthesia, radial arterial line was secured on the right side with 20 gauge cannula for monitoring, left hand radial was secured with 6F radial sheath. 14F right femoral sheath was placed and TEVARwas done under fluoroscopic guidance with a 38x38x150 cm endovascular graft. The patient was weaned off the ventilator and extubated the same day. He was mobilised and shifted to the ward on the first post-operative day. He was discharged on the third day post-procedure. No blood or blood product transfusion was needed.
TEVAR is an alternative to open surgery. It is a less painful procedure associated with shorter hospital stay and quicker recovery time.
Contraindications to TEVAR include inadequate proximal or distal seal zones, tortuosity, lack of vascular access options, or extremes of aortic diameter. It is also usually avoided in infected zones.

Dr. Gauranga Majumdar
Director - Cardiothoracic & Vascular Surgery
Medanta - Lucknow
In Focus
Association Between Tumor Necrosis Factor Inhibitors and Central Nervous System Demyelination
TNF inhibitors are pharmaceutical drugs that suppress the physiologic response to tumor necrosis factor (TNF), which is part of the inflammatory response and causative factor for diseases such as rheumatoid arthritis, juvenile arthritis, psoriatic arthritis, plaque psoriasis, ankylosing spondylitis, ulcerative colitis, and Crohn’s disease.
Due to the increase in usage of TNF blockers, several immune-mediated neurological complications such as transverse myelitis, optic neuritis, polycranial neuritis, multiple sclerosis, chronic inflammatory axonal polyradiculoneuropathy, and small-fiber polyneuropathy are being recognized[1]. However, the origin of these adverse reactions is debatable. TNF blockers may also increase the risk of viral, bacterial and fungal infections including rare infections like Progressive Multifocal Leucoencepathlopathy (PML).
Case Study
45-year-old patient with Crohn’s disease and AnkylosingSpondylosis on disease-modifying drugs (Methotrexate 25 mg weekly and Adalimumab 40 mg S/C bi-weekly) presented with complaints of acute onset of dizziness along with vomiting, right side weakness and change in voice with slurring of speech for four days. His examination revealed gazed evoked nystagmus, impaired gag reflexes, and severe right sided ataxia. His routine hematological tests, biochemistry and chest X-ray were normal. His MRI brain showed T 1 hypo intense, T 2 and FLAIR hyperintense signal changes in medulla, pontomedullary junction and dorsal pontine region with focal areas of restricted diffusion with minimal enhancement. Differential diagnosis of demyelinating lesions or infective lesions affecting brain stem was considered. However, his CSF study revealed normal findings making the infective possibilities unlikely.
Patient was started on IV Methylprednisolone.
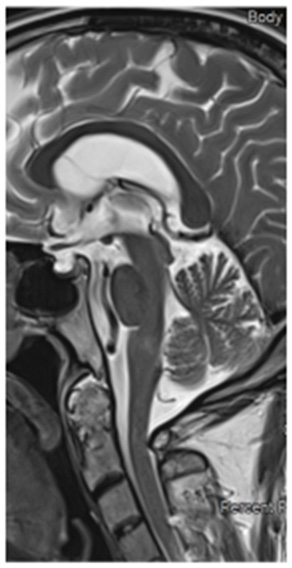

Pre-treatment MRI Brain T2 sagittalPost-treatment MRI Brain T2 sagittal
Patient responded well to the treatment and was discharged after five doses of IV Methylprednisolone. His follow up brain MRI after six weeks showed remarkable improvement confirming the diagnosis of brain stem demyelination.
Scientific Evidence
Review of medical literature suggests that patients treated with TNF inhibitors may develop symptoms due to CNS demyelination. E. Andreadou et al reported that four patients treated with TNF inhibitors developed symptoms suggestive of CNS demyelination[2]. All these patients showed improvement after stopping TNF inhibitors and starting IV Methylprednisolone. Appearance of lesions after initiating TNF inhibitors indicate a causal relationship between TNF inhibitors and demyelinating lesions. In some cases, demyelinating disorder persisted despite treatment discontinuation suggesting that TNF inhibitors can trigger the demyelinating process[3]. AlnasserAlsukhni et al reported that Adalimumab provoked multiple sclerosis in a patient with autoimmune uveitis with positive family history for multiple sclerosis (MS) and advised caution when using TNF inhibitors in patients with a family history of MS[4].
Conclusion
TNF inhibitors should be used after careful examination and relevant investigations must be performed to diagnose new symptoms. MRI should be considered in case of suspected CNS lesions at a low threshold. Prompt discontinuation of TNF inhibitors with the administration of IV steroid should be considered in case of CNS demyelination.
References:
- doi: 10.3823/339
- http://dx.doi.org/10.1155/2013/671935
- doi: 10.1093/rheumatology/kes375
- doi: 10.1155/2016/1423131
Dr.Ritwiz Bihari
Associate Director
Institute of Neuroscience
Medanta – Lucknow
TechByte
Polysomnography for Sleep Disorders
Polysomnography, also called sleep study, is a full-scale test done to diagnose sleep disorders. It examines sleep stages and cycles to catalog if or when sleep patterns are disrupted and why. In addition to diagnosing sleep disorders, polysomnography can also help begin or alter a patient’s treatment plan if they have previously been diagnosed with a sleep disorder.
Polysomnography is regularly done in Medanta’s sleep lab which has specialized equipment to record the patient’s breathing pattern, heartbeat, brainwaves, oxygen saturation levels, and movement of the eyes and limbs during sleep.
Polysomnography is performed in the following manner:
- A variety of sensors are taped to the body parts
to record brain waves, eye movements, muscle tone,
body movements, heart rhythm, and breathing
patterns overnight. No painful equipment (such as
needles) is used. - The oxygen content of the blood is measured
noninvasively with a pulse oximeter. - A trained sleep specialist is present for the entire study
duration to oversee the procedure as the set up
records the data.
Further treatment steps are taken based on the reports generated in the sleep lab. On an average, 45-50 sleep studies are conducted in Medanta every month.
Sleep medicine specialists and neurologists at Medanta recommend a sleep study whenever a patient shows signs of a sleep disorder such as:
- Falling asleep while driving
- Struggling to stay awake when inactive, such as when watching television or reading
- Facing difficulty concentrating at work, school, or home
- Experiencing performance problems at work or school
- Experiencing memory lapses
- Experiencing slow responses
- Experiencing emotional outbursts
- Taking frequent naps
Polysomnography is performed to diagnose and evaluatevarious kinds of sleep disorders such as:
Sleep Apnea
Sleep apnea occurs when a person’s breathing is interrupted during sleep.
Insomnia
Insomnia is a sleep disorder in which people have difficulty falling asleep or staying asleep. They may experience early morning awakening or unrefreshing sleep.
Restless Legs Syndrome
Restless legs syndrome is a sleep disorder prompting an extreme, often compelling urge to move the legs.
Circadian Rhythm Disorders
Circadian rhythm disorders stem from disruptions in the circadian rhythm, which is referred to as the “internal body clock” that controls the 24-hour cycle of biological processes in animals and plants.
Parasomnias
Parasomnias are sleep-related disorders that arise from rapid eye movement (REM) sleep or arousals from non-rapid eye movement (NREM) sleep.
Narcolepsy
Narcolepsy is a neurological disorder that happens due to reduced amounts of a neuropeptide called hypocretin in the part of the brain that regulates the sleep-wake cycle.
Sleep Disorders and Comorbid Medical Conditions
Sleep disorders and other medical ailments often coexist. Some medical conditions may lead to sleep disorders. Sleep disorders also can lead to several debilitating medical conditions.
Pediatric Sleep Disorders
Uninterrupted long durations of sleep are essential in infancy and early childhood, as the developing brain needs more time asleep than awake. Children with sleep disorders may experience a lack of adequate sleep time or poor sleep quality or both.
Sleep Disorders in the Elderly
Ageing leads to changes in sleep patterns, including increased light sleep, disrupted night time sleep, suffering from health conditions that adversely impact the sleep quality and quantity, sleeping less, and taking more daytime naps that may result in an irregular sleep-wake cycle.
Dr. Ashish Kumar Prakash
Senior Consultant
Respiratory and Sleep Medicine
Medanta - Gurugram






