THE EXCHANGE | Newsletter - Mar 2023
A Knowledge Sharing Initiative by Medanta
Complex Surgery to Treat Renal Cell Carcinoma with Inferior Vena Cava Thrombus and Double Renal Vein
Renal Cell Carcinoma (RCC) is the most common cause associated with inferior vena cava (IVC)
tumor thrombus accounting for 18% of all tumors associated with venous thrombi. The two
components of the thrombus include the tumor growing into the vein as a thrombus and the ‘bland’
thrombus - clotted blood - that develops as a result of hampered drainage. Management of RCC with
an associated IVC tumor thrombus can be technically challenging depending on the type and the level
of thrombus. Traditional classification of IVC thrombi include Level 1 as within 2cm from the renal
ostium, Levels 2, 3 and 4 as below hepatic veins, between hepatic veins and diaphragm, and above
the diaphragm, respectively.
The gold standard treatment includes a radical nephrectomy with regional lymph node dissection and
IVC thrombectomy. Certain pre-operative considerations for this major surgery include anticoagulation
to lower the risk for pulmonary embolism, pre-operative angioembolization, and availability of a
multidisciplinary team comprising of cardiothoracic and vascular surgeons.
Case Study
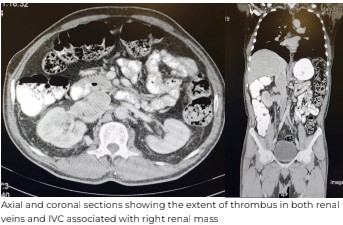
A 57-year-old male with diabetes, hypertension, hypothyroidism and chronic kidney disease
presented to Medanta-Gurugram with bilateral swollen feet and fever of unknown origin. He had an
incidental finding of a right renal mass, and, on physical evaluation, he was found to have bilateral
varicocele as well. His creatinine was 1.5 mg/dl with a hemoglobin of 8.8 g/dl. Initial ultrasound
revealed a right renal mass, followed by a CT scan, that revealed a large heterogeneously enhancing
mass, 7.6cmx5.3cmx8.2cm in size arising from the interpolar region of the right kidney, that had two
renal veins. This mass was extending into the renal sinus, both the right renal veins and contiguously
into the IVC for a length of 7cm, and a width of 4.2cm into the intrahepatic IVC below the hepatic
veins. Multiple enlarged collaterals were also seen. Hence, the patient was advised surgery, and he
underwent an open right radical nephrectomy with Level 2 IVC thrombectomy.
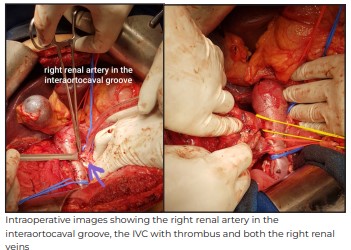
Intraoperatively, a subcostal chevron incision was given and after the initial mobilization of the colon
and the duodenum, IVC was exposed and the dissection carried out superiorly to take control of
vessels draining into the caudate lobe to gain some extra infra-hepatic IVC length. The right renal
artery was carefully dissected in the inter-aortocaval groove and ligated along with the lumbar veins.
Once all the vessels were exposed, sequential clamping was performed - infrarenal IVC, the left renal
vein and the suprarenal IVC. This was done very carefully to prevent dislodging of the thrombus.
Next, both the right renal vein openings were incised circumferentially and the incision extended onto
the antero-lateral surface of the IVC. The thrombus was excised en-bloc along with the kidney. The
IVC was flushed with heparinized saline and was carefully closed with 4-0 prolene sutures and the
clamps were released in the same order as they were applied.
The total intraoperative time was 210 minutes with a blood loss of 300 ml. The patient had an
uneventful post-operative recovery. He was observed overnight in a high-dependency unit and was
allowed clear liquids orally after eight hours. He was ambulated with support on Day 2 post-surgery
and was put on a semi-solid diet. His biochemical parameters remained stable with a marginal
increase in creatinine levels to 1.9 mg/dl. He was discharged by Day 5 on a normal diet.
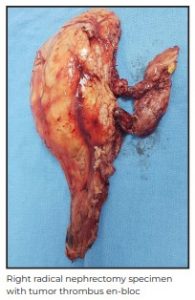
Histopathology revealed a right renal cell carcinoma pT3b N0, Grade 2
and thrombus positive for malignancy. Patient had regular follow up visits and at the end of two years, he is recurrence free as evidenced by interval cross-sectional imaging.
This case highlights the technical nuances and intraoperative meticulous steps that need to be
followed in this major surgery to prevent devastating complications, such as thrombus
dislodgement, pulmonary embolism, major hemorrhage and potential mortality.
Dr. Pankaj Wadhwa
Senior Director - Urology
Kidney and Urology Institute
Medanta – Gurugram
Medanta@Work
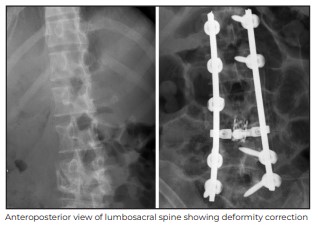
Post Tubercular Healed Severe Kyphotic Deformity with Altered Gait Treated Surgically
Pott's Spine accounts for about 2% of all cases of tuberculosis (TB), 15% of extrapulmonary cases
and 50% of skeletal TB cases. Clinically, it presents with constitutional symptoms, including back
pain, tenderness, paraplegia/ paraparesis, and kyphotic / scoliotic deformities. Most of the time, the
disease is restricted to the disc space with the collapse of vertebral body, but it can span to multiple
levels causing widespread bone destruction and consequently an unstable spine with deformity,
mainly kyphosis. It is not very uncommon to see such patients with advanced disease, especially in
rural areas where patients do not have access to timely intervention, initiation of anti-tubercular
therapy and surgical correction of the deformity. Such healed deformities of the spine present with
surgical challenges and might be associated with paraplegia, both in the pre-operative period and
also, unfortunately, post-surgical correction.
Case Study
A 24-year-old female presented at Medanta-Lucknow with stooped forward gait and a sharp deformity
over lower lumbar for the last six months. She had a history of lower back pain, which was insidious in
nature and gradually progressive for the last nine months. Initially, she responded to local treatment
and analgesics, but the pain started to worsen with prominence during the night, causing disturbed
sleep. There were multiple episodes of rise in body temperature towards the evening, associated with
sweating and loss of appetite. She also reported a history of significant weight loss – about 8kgs in
three months.
At the time of presentation, the patient was significantly cachectic and weighed only 38kgs. There was
generalized muscle wasting; she walked with her hands rested on the knees and had a stooped
forward posture. There was a prominent knuckle deformity around dorso-lumbar spine; all the
movements of the spine were painful. Neurologically, her sensory and motor assessment was normal.
Her bowel and bladder functions were also normal.

At another centre she had undergone a series of investigations, including a magnetic resonance
imaging (MRI) of the spine. Her initial radiographs of the spine showed spondylodiscitis at L3-L4 with
a kyphosis of 25 degrees. Her radiographs of lumbosacral spine were repeated at Medanta-Lucknow.
It was found that the kyphosis had progressed to 40 degrees, which did not correct on extension. The
CT scans showed extensive bone destruction with a kyphoscoliotic deformity around L3-L4. The MRI
scans showed extensive soft tissue component in the epidural space with pre- and para-vertebral
collections around L4.
She was diagnosed with post-tubercular sequelae at L3-L4 with severe kyphoscoliotic deformity. We
planned to do a thorough debridement of the dead and necrotic tissue and bone, collect biopsy
samples and attempt to correct the deformity without jeopardizing the neurological status.
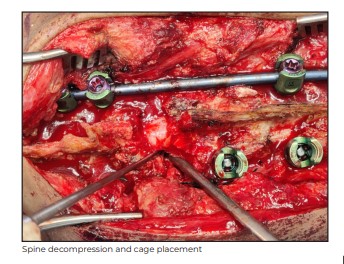
Intraoperatively, as the epidural space was opened, around 40ml of abscess was found, which was
collected for culture and drug sensitivity, and all the dead bone was removed. L4 was found almost
fully collapsed and a corpectomy was done. We got fixation points, both above and below the
involved level, by inserting pedicle screws. A major challenge was to restore the height of L4. The L4
and L5 nerve roots were too close to each other, which hindered putting a mesh cage inside. The
nerve roots could not have been sacrificed and hence, it was decided to do further bone resection
circumferentially to get that space in front of L4. Finally, the mesh cage was successfully positioned in
place of L4 vertebra, jacking it up to restore the height and correcting the kyphotic deformity.
The surgery was uneventful with good clinical outcome. Postoperatively, the patient had normal
neurological status and maintained all vital parameters. She was restricted to bed for two weeks and
was mobilized after her wounds had healed with the help of a walker.
Her postoperative radiograph showed correction of deformity to 10 degrees from the earlier 40
degrees at the time of presentation. The abscess culture and genetic experts confirmed the TB as
sensitive to first-line of drugs. At her two-month follow up, the patient showed clinical improvement, had gained weight and was walking pain-free.

The case highlights the importance of prompt diagnosis of spinal TB and alertness towards
development of any spinal deformity.

While Pott’s Spine is primarily a disease requiring proper and monitored treatment for at least one year, any deformity that is developing needs to be addressed promptly to prevent further morbidity. Surgical treatment options significantly improve patient outcomes, and are now well accepted.
Dr. Swetabh Verma
Consultant - Spine and Orthopaedics
Institute of Musculoskeletal Disorders and Orthopaedics
Medanta – Lucknow
TechByte
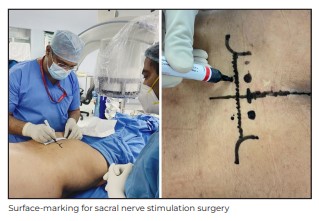
Sacral Nerve Stimulation for Neurogenic Bladder
Losing control over one’s ability to urinate can be emotionally and socially devastating. This was the
circumstance of a 54-year-old male who presented to Medanta-Gurugram. He was unable to pass
urine due to advanced spinal arachnoiditis-induced neurogenic bladder. The patient had been
suffering from a neurogenic bladder for more than five years and had not experienced any significant
relief or improvement from the medications, pelvic exercises and behavioral therapy. His quality of life
was severely impacted and punctuated by suicidal thoughts.
The patient underwent thorough clinico-radiological evaluation. Thereafter, he was advised an
ingenuous neuro-modulation therapy known as Sacral Nerve Stimulation (SNS) to correct his urinary
malfunction.
SNS is a neuromodulation therapy of the sacral nerves to modulate the reflexes that influence the
urinary bladder, sphincter and pelvic floor. It acts like a pacemaker and utilizes mild electrical pulses
to improve or restore normal voiding function. It is indicated for patients suffering from neurogenic bladder due to a plethora of neurological, urological and/or gynaecological causes, who have failed or
did not respond to conservative therapy, such as medications, behavioural therapy, and pelvic
exercises. Up to 30%-50% of all neurogenic bladder patients are non-responsive to conservative
therapy. Additionally, more than 90% patients who initially respond to conservative treatment become
non-compliant in about 24 months. In all such patients, SNS therapy is being seen as an effective
solution.
SNS therapy works for urinary urgency-frequency, incontinence and non-obstructive retention. The
mechanism of action is multifactorial; it is hypothesized that sacral nerve stimulation works via
modulation of spinal and supra-spinal reflexes through afferent signaling rather than direct motor
stimulation.
There is an initial trial period to assess the viability of SNS therapy. During the trial procedure
performed under local anasthesia, the right S3 nerve (preferable nerve of choice) is negotiated
through the appropriate sacral foramen under fluoroscopic guidance and stimulated for appropriate
motor and sensory reponses, confirming which the SNS electrode is implanted and secured to an
external stimulation system for next 3-7 days. Only those patients who experience at least 50%
improvement in their symptoms, during the trial period, are given a final SNS implantation.

During the trial period, our 54-year-old male patient experienced an improvement of more than 70% in
his symptom of urinary retention caused by a neurogenic bladder with more than 90% reduction in the
volume of post-void residual urine in the urinary bladder as assessed by ultrasound of kidneys,
ureters, and urinary bladder (KUB). Subsequently, he underwent implantation of a permanent SNS
pulse generator system as the next step.


The procedure went well with good clinical outcome. Patient was discharged on Day 3 of the
procedure and is doing well just like other satisfied patients who have previously undergone this
surgery at Medanta.
Dr. Anirban Deep Banerjee
Associate Director – Neurosurgery
Institute of Neurosciences
Medanta - Gurugram
Kudos

Congratulations Dr. V.P. Singh (Chairman, Institute of Neurosurgery, Medanta, Gurugram) on being
appointed the President of the Indian Society of Paediatric Neurosurgery – a body of country’s top neuro-
experts dedicated to advancing paediatric neurosurgery and knowledge exchange.
Welcome on board
Dr. Thekkinedath Joseph Antony
Director and HOD - Neonatology and NICU
Medanta - Gurugram
Neonatologist with over four decades of experience and expertise in neonatal
ventilation (conventional/high frequency), total parenteral nutrition, phototherapy,
exchange transfusions and peritoneal dialysis. He specialises in management
of complex medical problems in preterm newborns and critically ill neonates.
Dr. Preeti Rastogi
Director and HOD
Obstetrics and Gynaecology
Medanta - Gurugram
Gynaecologist and high-risk obstetrician with over 25 years of experience and
expertise in painless deliveries, benign gynaecological disorders, peri and post
menopausal care. She also specialises in laparoscopic and robotic surgery such as
hysterectomy, myomectomy, ovarian cystectomy, vaginal and pelvic reconstruction surgeries.
Dr. Neha Gupta
Senior Consultant
Obstetrics and Gynaecology
Medanta - Gurugram
Gynaecologist with expertise in minimally invasive gynaecology (laparoscopic
and hysteroscopic surgeries), high risk pregnancy care and delivery in addition to
gynae endocrinology (infertility, PCOS).
Dr. Pooja Mittal
Senior Consultant
Obstetrics and Gynaecology
Medanta - Gurugram
Gynaecologist with expertise in infertility, high risk pregnancy and delivery, complex
gynaecological surgeries in addition to laparoscopic procedures.
Dr. Sarita Sharma
Senior Consultant
Gynaecology and Gynae Oncology
Medanta - Patna
Gynaecologist with expertise in high risk obstetrics, complex gynaecological surgeries
including gynaecological oncology, robotic, laparoscopic and hysteroscopic surgeries.
Dr. Ankit Gupta
Consultant - Neonatology and NICU
Medanta - Gurugram
Neonatologist with expertise in managing extremely preterm neonates including
nano preemies, critical medical and surgical newborn cases in addition to neonatal
transport.
Dr. Kanika Singh
Consultant - Paediatrics and Clinical Genetics
Medanta - Gurugram
Paediatrician and clinical genticist with expertise in paediatric genetics and
metabolic disorders, genetic counselling, antenatal counselling, fetal anomalies,
recurrent pregnancy loss, adult onset genetic disorders in addition to cancer and cardiac genetics
Dr. Naresh Panwar
Consultant - Neurosurgery
Medanta - Lucknow
Neurosurgeon with expertise in treating various neurological disorders and spine
diseases. He specialises in skull base surgery, neuro endoscopy, minimally invasive spine
surgery, cerebro-vascular neurosurgery and deep brain stimulation.
Dr. Priyanka Karnani
Consultant - Neonatology and NICU
Medanta - Gurugram
Pediatrician and neonatologist with expertise in managing level 3 NICU including
ventilation, complex neonatal procedures and high risk developmental follow-up of
newborns discharged from NICU.
Dr. Ruchi Dhall
Consultant - Neonatology
Medanta - Gurugram
Neonatologist with expertise in neonatal ventilation, nutrition of babies with
extremely low birth weight, developmental follow-up of high risk newborns,
management of various medical and surgical conditions in neonates.
Dr. Deepak Kumar
Consultant - Nephrology and Kidney
Transplant Medicine
Medanta - Patna
Nephrologist with expertise in kidney transplant, transplant immunology, critical
care nephrology, interventional nephrology and glomerulonephritis.
Dr. Amrita Swati
Associate Consultant - Pulmonology
Medanta - Patna
Pulmonologist with expertise in diagnosing and treating obstructive lung diseases,
interstitial lung diseases, pneumonia, tuberculosis, pleural diseases and sleep
related disorders. She also specialises in pulmonary critical care and bronchoscopy.
Dr. Tejasvini Vaid
Associate Consultant - Medical Onco and
Haemato Oncology
Medanta - Gurugram
Clinical hematologist with expertise in benign hematology, hemato-oncology and
stem cell transplantation
Dr. Kumar Pankaj
Associate Consultant - Urology and Kidney
Transplant Surgery
Medanta - Indore
Urologist with expertise in laser surgeries for kidney stones, endourology (urolithiasis
and prostate), reconstructive urology and laparoscopic surgery.
Dr. Richa Garg
Associate Consultant - Breast Services
Medanta - Gurugram
Breast surgery specialist with expertise in breast disease management (benign and
cancer), sentinel node biopsies and breast cancer surgeries
Dr. Madduri Veera Sekharaiah
Associate Consultant - Clinical and Preventive Cardiology
Medanta - Gurugra
Cardiologist with expertise in treating all forms of cardiac illnesses, including
coronary artery disease, valve diseases, cardiomyopathies, etc.
Dr. Shiepra
Associate Consultant - Dental Sciences
Medanta - Patna
Dentist with expertise in managing maxillofacial trauma, head and neck
cancer, oral prophylaxis, dental restorations, dental extractions and impactions in
addition to full mouth restoration, dental implant placement and minor oral surgical procedures.






