THE EXCHANGE | Newsletter - Jun 2023
Asia’s First Tricuspid Valve Clipping Treatment Done at Medanta Gurugram

A 57-year-old Nepali monk was diagnosed to have chronic liver disease after he suffered a Hepatitis C virus infection in 2008. On two occasions - once in 2011 and then again in 2018 - he developed gastrointestinal bleeding and decompensation with ascites. Both these episodes were managed well at Medanta - Gurugram with medication. He was also diagnosed with atrial fibrillation and severe tricuspid regurgitation with mild pulmonary hypertension.
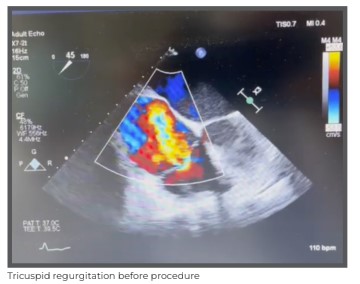
In May 2023, he again presented to Medanta - Gurugram with severe decompensated liver disease with bilirubin reading of 10mg/dl, grade-3 oesophageal varices post-endoscopic variceal ligation (EVL), mild portal hypertensive gastropathy, ascites (fluid collecting in the abdomen) and hepatic hydrothorax requiring liver transplantation. However, the patient’s condition - severe tricuspid regurgitation - made him unfit for transplantation.
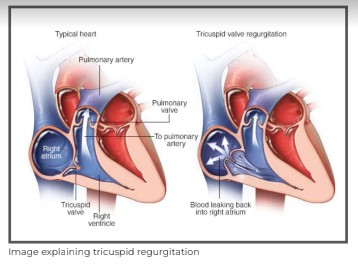
Tricuspid regurgitation is a condition that occurs when the tricuspid valve in the heart fails to close properly, leading to blood flowing back into the right atrium. This can cause a variety of symptoms, including fatigue,
shortness of breath, heart palpitations and ascites. Severe tricuspid regurgitation has been associated with hepatic congestion and can progress to liver cirrhosis. Additionally, presence of severe tricuspid regurgitation is a contraindication to liver transplant surgery. Although, an isolated tricuspid valve surgery is done occasionally, it is associated with high mortality – highest among all valve interventions; options for percutaneous interventions are still at a nascent stage.
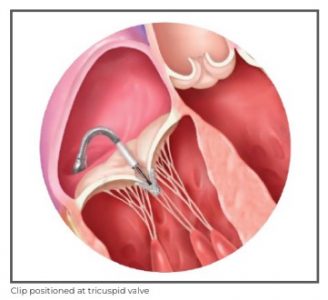
Tricuspid valve clipping treatment using MitraClip is a new, minimally invasive procedure that has shown promising results in treating tricuspid regurgitation.

During the procedure, a small clip is placed on the leaflets of the tricuspid valve to help it close properly.
While tricuspid clipping treatment is still a relatively new procedure, it has the potential to greatly improve the lives of those suffering from tricuspid regurgitation.
Unlike traditional surgeries, tricuspid clipping treatment does not require the chest to be opened up, and recovery time is much shorter.
Studies have shown it to be safe and effective with patients reporting significant improvement in their symptoms.
Hence, for our patient, following a multidisciplinary team accord, we decided to perform a tricuspid valve clipping procedure - the first ever in Asia.
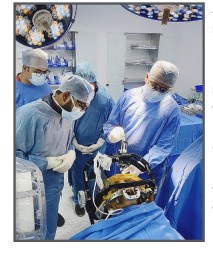
The procedure was performed under general anaesthesia, navigated by advanced 3D echocardiographic imaging. It was completed in an hour with the placement of two clips and the tricuspid regurgitation was reduced to mild leak from a severe leak. The patient was extubated on the same day and stabilised for the next few days. On Day 8 of the cardiac procedure, he underwent a successful liver transplantation surgery at Medanta - Gurugram.
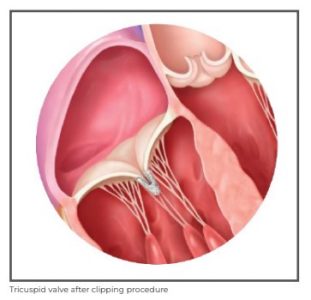

The patient has recovered well and has reported significant improvement in his quality of life.
Dr. Praveen Chandra
Chairman - Interventional and Structural Heart Cardiology
Heart Institute Medanta - Gurugram
Dr. Nagendra Singh Chauhan
Senior Director - Interventional Cardiology
Heart Institute Medanta - Gurugram
Dr. Manish Bansal
Senior Director - Clinical and Preventive Cardiology
Heart Institute Medanta - Gurugram
Infocus
Directional and Brain Sensing - Coupled Brain Pacemaker Surgery
A Game Changer in the Treatment of Parkinson's Disease
Deep Brain Stimulation (DBS) surgery, also known as brain pacemaker surgery, is an established therapeutic option for improving quality of life of patients suffering from certain advanced disabling diseases, including a spectrum of movement disorders such as Parkinson’s disease, essential tremor, dystonia in addition to intractable adult epilepsy and OCD.
The essence of DBS surgery is precision. In this regard, ‘Directional DBS and Brain Sensing’ have emerged as game changers. Unlike conventional DBS that only allows neuromodulation in one direction, the segmented electrodes (leads) used in directional DBS help in steering brain stimulation of the specific region-of-interest in all three dimensions, thus significantly enhancing the focus and precision of therapeutic gains while minimising inadvertent side-effects.
Another promising technological aspect being explored is a real time brain-sensing biomarker-guided feedback analysis of the local field potentials by the brain pacemaker pulse generator itself, which would then automatically release a closed-loop anticipatory stimulation response, as and when needed, back to the brain so as to alleviate any unpredictable manifestations or symptoms of Parkinson’s disease as far as possible. This technology holds the promise of removing the need for frequent manual programming of the brain pacemaker by the doctor, which is mandatory after conventional brain pacemaker surgery.
Recently, at Medanta - Gurugram, North India’s first ‘Directional and Brain Sensing-coupled’ DBS system was implanted in a 70-year-old male patient suffering from incapacitating Parkinson’s disease for the last 15 years. This patient had developed severe camptocormia (Bent Spine Syndrome).
Camptocormia (from the Greek words “kamptein” meaning to bend and “kormos” meaning trunk) is a condition characterised by a distinct extreme forward bending of the spine while sitting, standing, walking that vanishes on lying down. A common association with Parkinson’s disease, camptocormia is hypothesised to be most probably caused by dysregulation of roprioceptive polysynaptic reflexes.
The results of Deep Brain Stimulation in Bent Spine Syndrome are heterogeneous. Overall consensus is that the improvement after DBS is inversely proportional to the duration of camptocormia and directly proportional to the pre-surgical severity of this non-fixed spinal deformity in patients of Parkinson’s disease.
Given the extremely advanced nature of the patient’s condition, we felt that the soul of DBS therapy for him would reside in its ability to precisely utilise the subthalamic homunculus with sub-milliletric accuracy and minimise the side-effects even in the long run. Therefore, we opted for ‘Directional and Brain Sensing-coupled' brain pacemaker surgery for this patient.
A month after the surgery, the patient has shown steady reduction in forward stooping, especially while sitting, and it is expected that the improvements in his quality of life will steadily build up with time.
Dr. Anirban Deep Banerjee
Associate Director - Neurosurgery
Institute of Neurosciences
Medanta - Gurugram
Medanta@Work
Clinically Challenging Management of Giant Pheochromocytoma
Pheochromocytomas (PCC) are highly vascularised tumours arising from the neural crest tissue; they may also arise from chromaffin cells/parasympathetic ganglion (e.g. carotid body, glomus tympanicum, glomus jugular, glomus vagale). PCCs are dark-coloured tumours because of oxidation and polymerisation of catecholamines by chromium salts. They commonly present in the fourth and the fifth decade of life, but can also present earlier in case of familial history.
The classic ‘Rule of 10’ for PCC is that 10% cases are malignant, 10% are bilateral, 10% are extra-adrenal and 10% are familial. These tumours can arise sporadically or can be inherited, associated with three syndromes – Multiple Endocrine Neoplasia type 2 (MEN 2), Von Hippel-Lindau disease and Neurofibromatosis type 1. The average tumour size in PCC is approximately 7cm, and the average weight is approximately 50gms to 200gms, but sometimes they may be bigger. Such tumours are called Giant PCCs and are a rarity. By definition, they are larger than 7cm with majority being cystic, and some can be benign. The clinical features of Giant PCC are so variable that it has been termed “The Great Masquerader”, but the most common symptoms include headache, profuse sweating, palpitations, tachycardia, episodic or sustained hypertension, anxiety and panic attacks, nausea, abdominal pain, paradoxical orthostatic hypotension, hyperglycaemia and micturition syncope. The clinical features are a result of catecholamine (dopamine, norepinephrine and epinephrine) secreted by the tumour or mass effect. Diagnosis of PCC requires checking for blood and urinary level of metanephrines and catecholamines.
Radiological evaluation includes MRI, CT scan, Epilepsy affects about 1% of the population in India and it is one of the leading causes of disability resulting from a neurological condition. Around 40% of these patients are very likely to have uncontrolled epilepsy i.e. Drug-Resistant Epilepsy (DRE) causing persistent seizures that continue despite adequate trial of two or more anti-seizure medications (ASMs).
DOTATATE PET scan and metaiodobenzylguanidine (MIBG) scintigraphy. Treatment involves doing an adrenalectomy after adequate optimisation as defined under the Roizen Criteria:
- No blood pressure >160/90mmHg should be evident for 24 hours before surgery
- For patients with orthostatic hypotension, readings >80/45mmHg should be present
- No ST-T (segment and wave) changes in electrocardiogram for at least 1 week
- No more than one premature ventricular contraction for every 5 minutes
Case Study
A 45-year-old male, non-diabetic and of moderate built presented to Medanta - Indore with complaints of pain in the left loin and a palpable lump in the left flank for past 15 days. He was also experiencing symptoms of gastric outlet obstruction over similar duration. On evaluation, he shared that he had been experiencing headaches, perspiration and palpitations for the last 2-3 months and had had 2 episodes of syncopal attacks. On examination, his blood pressure (BP) measured 260/100 mmHg, heart rate was 120 beats/min and abdominal examination revealed left lumbar and a hypogastrium lump that was bimanually palpable, firm to hard and non-tender.
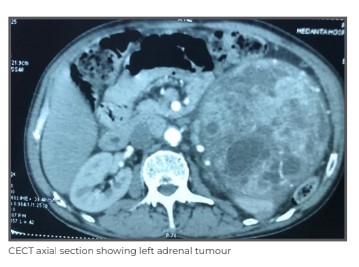
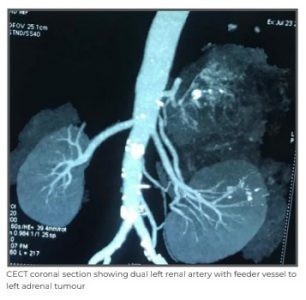
An abdominal ultrasound was done that revealed a retroperitoneal mass. Contrast enhanced computed tomography (CECT) of abdomen showed a huge adrenal mass of size 14cm*16cm. Blood investigations revealed haemoglobin (Hb) at 7 gm%, total leukocyte count (TLC) 11000/cumm, platelets 2.65 lakh/cumm, serum creatinine 1.1mg/dl, random blood sugar 320 mg/dl and urinary vanillylmandelic acid (VMA) 21 mg/24 hrs, while coagulation profile was within normal limits.

Based on the imaging and blood reports, the patient was diagnosed with Giant PCC and was counselled about the nature of disease with need for surgery involving a multi-specialty team, including a urologist, an endocrinologist, a cardiologist and an anaesthesiologist. Before surgery, the patient was hospitalised under the care of an endocrinologist and optimised for the procedure. He was started on Tab Prazosin 2.5 mg for alpha blockade. The dose was gradually increased up to 10mg over 2 weeks. In the last 2 days of the patient’s 10-day initial admission period, he was given Tab Metoprolol 25 mg once a day for beta blockade, and then discharged. He was re- hospitalised after 2 weeks and blood investigations were repeated revealing Hb 7 gm% with clinical examination results of BP 140/90 mmHg and pulse 78/min. In view of low haemoglobin count, 2 units of packed red blood cells (PRBC) were transfused over 2 days. A complete blood count (CBC) test was repeated and it showed improvement - Hb 9 gm%.
Satisfied with the results, the surgery and related complications were explained to the patient and his relatives. A high-risk consent was taken in view of the risk of intraoperative hypertensive crisis and stroke. The team arranged four units each of PRBC and fresh frozen plasma (FFP). The patient was started on all medications, as prescribed by the endocrinologist and cardiologist in addition to maintaining proper hydration and pre-operative fasting of 8 hours.
The principle for surgical management of PCC is “to remove the patient from the tumour” i.e. minimal to no-handling of the tumour. Splenic hilum, pancreatic tail and body along with left kidney were isolated. Adrenal vein was ligated first and the adrenal artery – directly originating from the aorta –identified, ligated and divided. Although the team took all precautions in keeping with the “no-touch technique” for the tumour, there were three intra-operative episodes of accelerated BP (reaching 240/120 mmHg) and heart rate shooting to 130/min.
These episodes were managed with Nitroglycerin (NTG) infusion, intravenous (IV) injections of Labetalol (4 mg) and pausing surgery till the patient became haemodynamically stable again. The tumour was resected in toto – BP 120/70 mmHg, pulse rate 100/min, central venous pressure (CVP) 4 mmHg. As soon as the adrenal vein was ligated, the systolic BP episode was managed with fast transfusion of 2 units of PRBC and 4 units of FFP. Norepinephrine infusion support was also given and BP slowly came to 130/80 mmHg with pulse rate at 78/min and CVP of 10 mmHg.

This was followed by arterial blood gas (ABG) analysis that showed Hb 8 gm%, potassium 2.5 mmol/lit and 500 ml expected blood loss. Potassium supplements were started intravenously at a rate of 4 ml/hr (40units in 40ml of saline - 1unit/ml) with insulin infusion already in place. Intra-operative urine output was 700 ml and the surgery lasted 4 hours. After the operation, the patient was shifted to the ICU with ionotropic support of injection norepinephrine and pressure-regulated volume control (PRVC) respiratory support – tidal volume (TV) 450 ml, respiratory rate (RR) 18/min, fraction of inspired oxygen (FIO2) 0.6, positive end-expiratory pressure (PEEP) 5. Third PRBC was started as the post-operative Hb was 8 gm%; BP was maintained at 130/80 mmhg, heart rate 88/min and CVP 12 mmHg. Injection norepinephrine was gradually tapered over 2 hours and finally patient was extubated after another hour. The patient’s remaining recovery in the ICU and the ward remained uneventful, and he was discharged on Day 5 of the procedure.
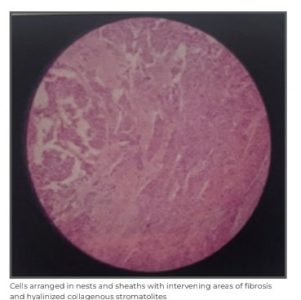
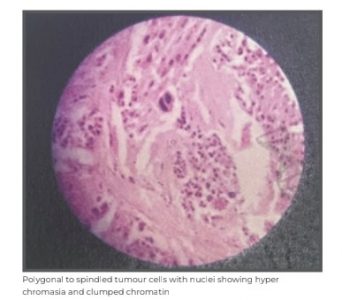
Histopathological examination showed composite PCC of adrenal gland and ganglioneuroma.
Dr. Ravi Nagar
Associate Director and Head - Urology and
Kidney Transplant
Kidney and Urology Institute
Medanta - Indore
Successful Salvage Surgery in Advanced Oral Cancer with Multiple Primary Cancers
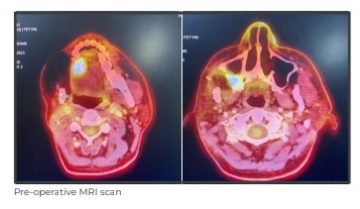
A 43-year-old male with a history of right buccal mucosa cancer for which he had undergone surgery and radiation therapy in 2019 was on regular follow up at Medanta - Lucknow. During one of his follow-ups in 2023, a PET scan was done to check for foul smell coming from his mouth and a persistent headache, which revealed two new second primary cancers – one in the tongue and the other in low infratemporal fossa (ITF). Since the patient had a minimal mouth opening pertaining to his previous treatment, it even made the visualisation of the disease difficult. The PET scan indicated two F-fluorodeoxyglucose (FDG) avid lesions – one in the right lateral tongue and another in the supero-medial aspect of the maxillary sinus wall extending to lower half of pterygoid plates.
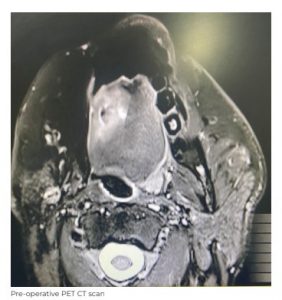
Simultaneously, we planned an MRI to look for the extent of the tongue lesion and high ITF peri neural invasion. We used a CT-guided biopsy to establish disease in the ITF. Initial investigations showed that a surgical resection was achievable, but reconstruction would be highly complex.

A surgical attempt to resect with an oncologic safe margin in a post-operative, post-radiation patient with minimal mouth opening is challenging; the effect of radiation on neck vessels and two completely separate sites of primary defect alsomake the reconstruction difficult. Hence, in case of such recurrences, it is important to counsel the patient about survival. It is also important for the treating surgeon to evaluate their decision making for the way forward. Whether or not to operate in such cases is defined not only by the surgeon’s calibre to resect, but also eclipsed by their potential to reconstruct.
In this case, we were aware that we might not be able to reach an oncologic safe margin and that reconstruction at two separate surgical sites would require two different free flaps. Considering a high ITF stage-4 disease versus the young age of the patient, even a 30%-40% chance of 5-year survival was worth striving for.
After counselling the family, we reached a unanimous decision to operate. Intraoperatively, he underwent right subtotal maxillectomy along with right extended hemiglossectomy through an angle split incision after raising a cheek flap. We were able to achieve a good resection with a considerable margin, but ended up with a huge defect to reconstruct. The gross defect measured 6.5cmx4cmx5cm and included maxilla, buccal mucosa and the tongue.



The initial plan for reconstruction was a double free flap, using free ALT flap to close the ITF defect followed by free radial forearm flap for tongue reconstruction. Following left neck dissection and identification of sizable vessels on opposite side for anastomosis in the neck, we decided to proceed with the ALT flap plan. The flap is often harvested on the descending branches of the lateral femoral circumflex artery and on its distribution territory the skin paddles are designed.
We found two strong direct perforators to the overlying skin paddles, which, with meticulous dissection, were separated helping us island overlying skin paddle. One half of the flap was used to reconstruct buccal mucosa and the other half for tongue. The flap was ipsilaterally anastomosed and a satisfactory reconstruction with good clinical outcome was achieved.


Considering large defects and a bulky flap, which presents immediate post-operative airway obstruction, difficulty swallowing and chances of aspiration, the patient underwent tracheostomy and was observed in the ICU for post-operative care. The patient was discharged from the hospital on Day 10 of the surgery. In post-operative week 3, he was able to vocalise and swallow.
Patient further underwent adjuvant radiation, which he tolerated well.
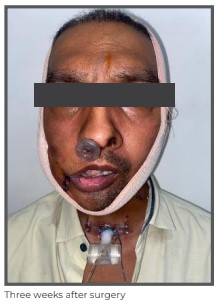
The patient, who was advised p a l l i a t i v e chemotherapy as the resection and reconstruction in his case looked far-fetched, is now disease-free and continues to be on follow up.
Dr. Vivekanand Singh
Director - ENT and Head & Neck Surgery
Head and Neck Oncology, Cancer Institute
Medanta - Lucknow
Dr. Piyush Sinha
Consultant - Head & Neck Oncology
Cancer Institute
Medanta - Lucknow
Welcome Onboard
 Dr. Sharad Tandon
Dr. Sharad Tandon
Director - Clinical and Preventive Cardiology
Medanta - Gurugram
Cardiologist with expertise in providing high-precision TEE- guidance for critical cardiac interventions and surgeries, including balloon mitral valvotomy, closure of atrial septal defect device, balloon atrial septostomy, TAVR, TMVR and LAA occlusions. He specialises in treatment of heart failure.
 Dr. Geetanjli Behl
Dr. Geetanjli Behl
Senior Consultant - Fetal Medicine
Medanta - Gurugram
Fetal medicine expert with proficiency in pregnancy scans - NT scan, anomaly scan, fetal Echo, multiple pregnancy scan, growth and Doppler scan, genetic counseling, pre-pregnancy and high-risk pregnancy counseling in addition to fetal procedures including amniocentesis, chorionic villous sampling, multifetal
reduction and intrauterine blood transfusion.
 Dr. Prakash Kumar
Dr. Prakash Kumar
Senior Consultant - Plastic,
Aesthetic and Reconstructive Surgery
Medanta - Patna
Plastic surgeon with expertise in hand and microvascular surgery, trauma reconstruction, onco
reconstruction, and aesthetic surgery.
 Dr. Anshul Patodia
Dr. Anshul Patodia
Consultant - Electrophysiology
and Pacing
Medanta - Gurugram
Cardiologist with expertise in performing simple as well as complex RF ablation of atrial and
ventricular arrhythmias, including 3D mapping. He specialises in device implantation such as dual
chamber pacemakers, automatic implantable cardioverter defibrillator (AICD) and cardiac resynchronisation therapy with defibrillator (CRT-D) in addition to conduction system pacing.
 Dr. Shahzeene Dhuria
Dr. Shahzeene Dhuria
Associate Consultant - Clinical
Immunology and Rheumatology
Medanta - Lucknow
Immunologist and rheumatologist with expertise in treating arthritis (rheumatoid, spondyloarthritis,
osteoarthritis, gouty arthritis), connective tissue diseases, inflammatory myopathies and vasculitis. She also specialises in procedures, including intra-articular and soft tissue injections, nail-fold capillaroscopy,
and biological usage in patients of autoimmune diseases.
 Dr. Yogendra Kumar Verma
Dr. Yogendra Kumar Verma
Associate Consultant - Neurology
Medanta - Indore
Neurologist with expertise in performing neuro-intervention procedures, such as mechanical
thrombectomy, carotid and vertical artery stenting, intracranial stenting, aneurysm coiling, AVM/
DAVF embolisation. He specialises in the treatment of movement disorders, neuromuscular
disorders, headaches, epilepsy, stroke, and cerebrovascular disorders.
 Dr. Sanjay Kumar
Dr. Sanjay Kumar
Associate Consultant - Plastic Surgery
Medanta - Patna
Plastic surgeon with expertise in reconstructive surgery related to trauma and cancer in addition to
cosmetic surgery.
 Dr. Ravi Bilunia
Dr. Ravi Bilunia
Associate Consultant - Plastic,
Aesthetic and Reconstructive Surgery
Medanta - Indore
Plastic surgeon with expertise in microvascular surgery, maxillofacial surgery, post-burn and post-
trauma reconstruction, cosmetic surgeries including breast augmentation and reduction, gynaecomastia, liposuction, rhinoplasty, blepharoplasty and aesthetics, such as fillers, botox, thread lift, hair transplant, PRP,
growth factor, scar and tattoo removal. He also specialises in AV fistula creation for dialysis and congenital defect management of cleft lip and palate, syndactyly, microtia and hypospadias.
 Dr. Ashutosh Prasad Tripathi
Dr. Ashutosh Prasad Tripathi
Associate Consultant - Interventional
Cardiology
Medanta - Gurugram
Interventional cardiologist with expertise in percutaneous transluminal coronary angioplasty (PTCA), chronic total occlusion (CTO) intervention, intravascular ultrasound (IVUS) imaging, implantation of temporary
and permanent pacemaker, implantable cardioverter defibrillator (ICD), intra-aortic balloon pump (IABP),
pericardiocentesis, 2D ECHO, and stress tests.
 Dr. Apurva
Dr. Apurva
Associate Consultant - Dental Sciences
Medanta - Patna
Dentist with expertise in the management of dentofacial anomalies such as protruded upper or lower jaw, corrective orthodontic treatment of cleft lip and palate in addition to alignment or correction of teeth irregularities with developmental malocclusion in children or adults.
 Dr. Ruchika Tahilyani
Dr. Ruchika Tahilyani
Associate Consultant - Gynaecology and
Gynae Oncology
Medanta - Lucknow
Obstetrician and gynaecologist with expertise in maternal and fetal medicine in addition to high-risk pregnancy management. She specialises in antenatal ultrasounds, invasive procedures like amniocentesis
and chorionic villus sampling for fetal abnormalities, genetic counselling and further management.






