THE EXCHANGE | Newsletter - Dec 2023
Medanta’s efforts to deliver high quality patient care and safety have won Medanta - Patna a seal of approval from the National Accreditation Board for Hospitals & Healthcare Providers. The recognition is a testament of our commitment towards constantly pursuing clinical excellence.
We will continue to deliver advanced healthcare through multi-disciplinary teams of experienced doctors and latest medical technology in a safe environment.
Spotlight
Advanced NICU Ambulance and Child Development Centre Launched at Medanta Lucknow
On the occasion of National Newborn Week, Medanta - Lucknow launched two new facilities –a Neonatal Intensive Care Unit (NICU) ambulance for immediate transfer of sick and premature babies, including at birth, and the other a Child Development Centre that will specialise in addressing the overall health and development needs of at-risk newborn babies and specially-abled children.
The dedicated NICU ambulance is an advanced neonatal transport vehicle equipped to manage newborns in need of specialised critical care. It has state-of-the-art equipment and specially trained staff - a multidisciplinary team of experts trained in the use of advanced technology - for newborn babies ensuring they get care equivalent to a Level-3 NICU even while they are in transit.
On arrival at the hospital, the newborns will be shifted to the Level-3 NICU which is the first-of-its-kind in Uttar Pradesh and has been set-up to care for premature babies.
The neonatal transport service is available 24x7 and has facilities, including total body cooling therapy, heart and lung monitors, high frequency and conventional ventilators, nitric oxide, blanket warmers, enhanced vehicle hydraulics to ensure a smooth ride, ambient lighting to enhance relaxation, phototherapy and, drugs and defibrillators.


The Child Development Centre launched at Medanta - Lucknow has expert doctors and staff to take care of high-risk newborn babies, including specially-abled children who may have Autism, Attention Deficit Hyperactivity Disorder (ADHD), speech delay, seizures or other brain-related issues. The centre offers facilities, including child physiotherapy, occupational therapy, speech therapy, child neurology, etc. for timely intervention, and speedily offering multidisciplinary, optimal care for neuro-developmental delays in children.
Medanta@Work
Multiple Sclerosis with Myasthenia Gravis: An Unusual Case of Autoimmunity
Even though polyautoimmunity exists between different autoimmune diseases, the co-occurrence of multiple sclerosis (MS) and myasthenia gravis (MG) is rare. Autoimmune phenomenon is causative in both myasthenia gravis and multiple sclerosis. Although MS is primarily mediated by T Lymphocytes and MG primarily involves the destruction of the neuromuscular junction by antibodies, there is evidence that both cell-mediated and humoral immunity are involved in the pathogenesis of both these diseases. Different studies have shown T cell dysfunction and B cell involvement in the pathogenesis of both these diseases.
Previous case reports were mainly of female patients who had a mild presentation of MG either prior to or after diagnosis of MS. In this case, we report a unique male patient with a previous diagnosis of MS who presented with symptoms of MG after 15 years of initial diagnosis.
Case Study
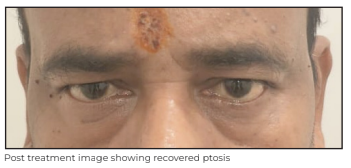
A 51-year-old male presented to Medanta - Lucknow with complaints of blurred vision, diplopia, and drooping of both eyelids with no fluctuating characteristics for the last one month. He did not have any generalised weakness or walking difficulty.
He had a history of hypothyroidism and relapsing-remitting multiple sclerosis (RRMS) diagnosed in 2008 after the initial presentation of internuclear ophthalmoplegia (INO) and optic neuritis. He was on dimethyl fumarate (DMF) for the next six years, i.e. up to 2014, after which he did not have any other recurrence and stopped the treatment on his own. Considering it to be MS recurrence, his MRI with contrast of brain and spine was done, which showed no active lesion.
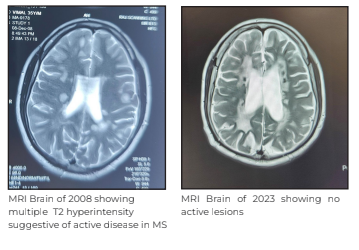
Further, he was taken up for comprehensive diagnostic check-up, which included panels for creatine kinase (CK), thyroid stimulating hormone (TSH), serum neuromyelitis optica (NMO) with myelin oligodendrocyte glycoprotein (NMO-MOG) antibodies, acetylcholine receptor (AChR) and anti-muSK (muscle specific kinase) antibodies, paraneoplastic, and autoimmune diseases. He was started on pulse-IV methylprednisolone after which the patient showed significant improvement in his ptosis. Later, his AChR antibody also came positive (6.42) and his repetitive nerve stimulation test (RNST) also showed decremental response in orbicularis oculi. He was started on oral steroids for immunosuppression with pyridostigmine and was given Rituximab for long-term management of both diseases. At his three-month follow-up, the patient was doing well with recovered ptosis in both eyes.

Discussion
The co-occurrence of MS and MG is rare. Previous studies suggest that a similar immunogenetic background creates a predisposition to susceptibility to these two diseases. But, different triggering and unknown genetic factors result in two different clinical diseases. MG can present before or after the diagnosis of MS, and the time for onset of this association may vary from one year to 28 years.
In literature review, we found approximately 30 patients who had co-occurrence of these two diseases. Cases of other demyelinating disorders other than MS, such as NMO, MOG and acute disseminated encephalomyelitis (ADEM), were excluded. Most patients were females with a mild clinical course of MG and MS. However, cases of primary progressive multiple sclerosis (PPMS) or MG crisis were rare. Few case reports also described the development of MG after treatment of MS with IFN-beta, glatiramer acetate and alemtuzumab.
It is not known whether immunomodulatory drugs are triggering factors in an already predisposed patient, or directly cause MG. Different immunological mechanisms and theories for loss of self-tolerance have been implicated in MG and MS. One of these theories is defects or dysfunction of T regulatory cells (Tregs), which function by suppressing the effector CD4+ T (Teff) cells that mediate autoimmune responses.
Conclusion
Co-occurrence of MG and MS is more frequent than expected by random association and the association may be underdiagnosed because of the possible overlap of symptoms, especially bulbar and ocular manifestations in which either MG or MS can mimic each other, leading to underestimation of the incidence of the combination.
Although MG is caused by autoantibodies to Ach receptors in neuromuscular junction, the mechanism underlying the autoimmune response appears to be initiated by activation of T lymphocytes. Alternatively, although MS is primarily mediated by T lymphocytes, there is some evidence that B cells and self-reactive antibodies play a role in the pathogenesis of MS as well. The enhanced understanding of T cell and B cell surface receptors and genes that are involved in the pathogenesis of MG and MS, needs further studies and clinical trials for developing more effective treatment options.
Dr. Vibhor Upadhyay
Associate Consultant - Neurology
Institute of Neurosciences
Medanta - Lucknow
Dr. Anup Kumar Thacker
Director - Neurology
Institute of Neurosciences
Medanta - Lucknow
Prophylactic Replacement of Ascending Aorta with Bicuspid Aortic Valve
Bicuspid aortic valve (BAV) is a common congenital abnormality in adults affecting 0.5%-2% of the population with a male preponderance of presentation in 3 males for every 1 female. While BAV itself may lead to isolated aortic valve disease – more frequently causing aortic stenosis than regurgitation or mixed lesion – 20%-40% of patients have associated aortopathies and aortic aneurysms. Aortic involvement can occur independently of valve function and pathology, most commonly involving the ascending aorta (AA), followed by the root, the arch and the descending aorta.
Prophylactic Aortic Surgery for BAV
The argument for prophylactic surgical intervention to replace the involved sections of the aorta gains credence based on the natural historical data for thoracic aortic aneurysms (rupture or dissection), substantial risk of aortic complications in dilated ascending aorta and aortic aneurysms.
The current indications for prophylactic aortic surgery for patients with BAV are:
• BAV without high-risk features with aortic root (ArR) or AA ≥ to 5.5cm.
• BAV with high-risk features or low estimated surgical risk (<4% risk of mortality) with ArR or AA ≥ 5.0 cm.
• BAV patients undergoing cardiac surgery for any cause, including aortic valve surgery, with AA or ArR ≥ 4.5cm.
Case Study
A 55-year-old male patient presented to Medanta - Ranchi with Class-III exertional dyspnea as per the New York Heart Association (NHYHA) Classification. Echocardiography (Echo) and basic investigations revealed BAV with severe calcific aortic stenosis. The chest X-ray showed what appeared to be exaggerated unfolding of the aorta, although the mediastinum did not appear remarkably widened. A computed tomography (CT) aortogram was done, which showed AA dilated to a maximal diameter of 4.9cm.
The sinuses of valsalva measured 3.1cm, ArR at the origin of innominate artery measured 3.7cm and descending aorta was 2.7cm.
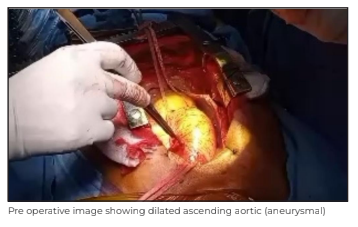
After getting the patient’s informed consent, he was taken up for surgery. We performed a median sternotomy. The pericardium was opened and the innominate vein and the AA were looped. As the arch of the aorta was curving back, and posteriorly rapidly, the innominate artery was cannulated to conduct a cardiopulmonary bypass (CPB) as it was more accessible, of a good size, and free of disease.
The rest of the cannulas and the CPB were done in the standard manner. Aorta was cross-clampled 2cm proximal to the origin of innominate artery and cardioplegic arrest was obtained by delivering cold del Nido cardioplegic solution, from cannulas placed in the ascending aorta antegradely and retrogradely through the coronary sinus. The AA was transected leaving a 2cm cuff at the sino-tubular junction (STJ). Aortic valve replacement was done with 20mm Miltonia bi-leaflet prosthesis. The STJ was sized and a 30mm woven polyester-coated graft with bovine collagen (Intergard/ Getinge) was selected. The graft was sutured first to the STJ and then to the digital aortic cuff with 5-0 polypropylene continuous sutured in a single layer. An aortic root cannula was placed in aortic graft for de-airing the heart; hot shot drugs were administered and the rest of the procedure was completed successfully as per the standard procedure.
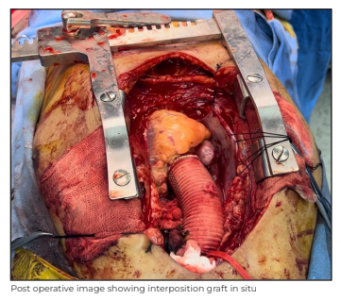
The patient had an uneventful post operative recovery and was discharged on Day 7 after the procedure. He was doing well on follow-up.
Key points:
1. Patients known to have BAV, even if free from aortic valve disease, require periodic imaging of the aorta by Echo, cardiac MRI or CT aortogram on account of frequent associated aortopathies. Interval of screening is determined on the basis of the presence of high-risk features, including:
- Degree and rate of progression of aortic disease
- Family history of aortic disease, sudden cardiac death or aortic dissection
2. Screening and surveillance is continued lifelong with periodic imaging if the aortic diameter is 4.0cm or more.
3. Prophylactic surgical intervention to replace the aorta is indicated when the aortic diameter reaches:
- 5.5cm for BAV with isolated aortopathy
- 5.0cm if associated with high-risk features
- 4.5cm for patient needing surgery for associated valve disease.
Dr. Balamurali Srinivasan
Associate Director
Cardiac Thoracic Surgery
Heart Institute
Medanta - Ranchi
TechByte
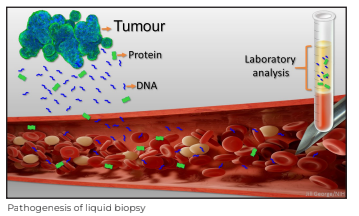
Liquid Biopsy: The Future of Cancer Diagnosis
Over the last few decades, the concept of precision medicine has dramatically changed the field of medical oncology. The introduction of therapies that can be tailored to meet the patient’s needs has significantly improved all measurable outcomes. Liquid biopsy is a revolutionary technique that is creating unexpected perspectives.
What is Liquid Biopsy?
A test done on circulating tumour cells or shed fragments of tumour DNA from a sample of blood to determine the gene signature or molecular portrait of a tumour is known as a liquid biopsy (LBx), or circulating tumour DNA assay (ctDNA).
For patients, the benefits of such solutions are evident: it provides ease of sampling; it is non- invasive; acceptable and repeatable. While cfDNA is DNA freely circulating in the blood that may or may not have originated from a tumour, ctDNA originates from tumours. ctDNA/ cfDNA and circulating tumour cells (CTCs) can be assayed using next-generation sequencing (NGS).
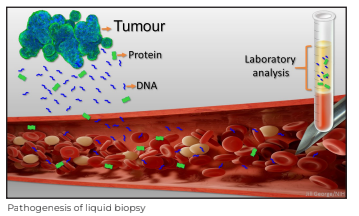
Why Liquid Biopsy?
Cancer is a cellular disorder characterised not only by its genetics but transcriptomic, proteomic expression patterns and cellular interactions. Liquid biopsy is driving an integrative approach to cancer diagnosis and therapeutic options.
ctDNA liquid biopsy solutions are currently approved as additional tools to the standard of care, and when results are negative, tissue testing is recommended, when available. The smaller the cancer, the smaller and less detectable the cancer signature in the blood. As any cancer grows, it sheds more DNA, more cellular debris and more cancer cells into the bloodstream, which eventually leads to the cancer spreading to distant organs.
The smaller the tumour, the higher the probability of a false negative result for a particular actionable mutation.
Advantages of Liquid Biopsy
• It is a minimally invasive procedure and can be applied to many body fluids (blood, urine, ascites, pleural effusion, etc.).
• Solves the issue of insufficient tissue for molecular analysis.
• Can be used for monitoring disease progression.
• Can be repeated for “real-time” follow-up of molecular changes during the disease course, i.e., driver mutation.
• Can be used to identify therapeutic targets without invasive biopsies.
• Minimal residual disease detection.
Limitations of Tissue Biopsy
• Represents only a spatial and temporal snapshot of the solid tumour.
• Sub optimal to represent tumour heterogeneity, especially when the tumour is not easily accessible or multiple tissue biopsies are not feasible.
• Small biopsies may not be sufficient for molecular analysis; this can occur in up to 15% of biopsy samples, as observed at Medanta - Gurugram.
• Decalcified tissue (e.g bone metastasis) causes significant DNA degradation such that it cannot be utilised for tissue-based molecular profiling.
• The overall turnaround time (TAT) for molecular analysis of a tumour, from scheduling the biopsy to histological analysis and finally molecular results, can take a significant amount of time that may impact therapeutic decision-making and clinical care.
Laboratory Test
NGS is emerging as a revolutionary approach for molecular testing. This cost-effective approach can analyse from ten to hundreds of genes from multiple patients at the same time. One recent study developed CAncer Personalized Profiling by deep Sequencing (CAPP-Seq). The CAPP-Seq method is capable of detecting ctDNA in all Stage II-IV non-small cell lung carcinoma patients and in 50% patients with Stage-I cancer. The specificity of the test was 96% for mutant allele fractions down to approximately 0.02%.
The adoption of liquid biopsy is accelerating and this is not more evident in non-small cell lung cancer (NCSCL). CAP/IASLC/AMP and ASCO recommend, in NSCLC, when tissue is limited and/or insufficient for molecular testing, a ctDNA assay can be used to identify epidermal growth factor receptor (EGFR) mutations.
It is also recommended that liquid biopsy be conducted at the time of initial diagnosis if the turnaround time for tissue biopsy is anticipated to be longer than 2 weeks.
Liquid Biopsy at Medanta
Medanta does liquid biopsy for NSCLC with an 11 gene panel using NGS, which can detect very low number of tumour cells with 0.1% of limit of detection. We are developing liquid biopsy for colon and breast cancers as well. With the new technology of digital Polymerase Chain Reaction (PCR) coming up, many customised panels and single genes can be tested with prompt results.
Dr. Dheeraj Gautam
Director - Laboratory Medicine, Pathology
and Blood Bank
Medanta - Gurugram
Dr. Rashi Sharma
Consultant - Molecular Histopathology
Medanta - Gurugram
In Focus
 Dr. Shoibal Mukherjee
Dr. Shoibal Mukherjee
Director - Medical Research
Medanta
We are pleased to welcome Dr. Shoibal Mukherjee to the Medanta Group as Director - Medical Research.
Dr. Mukherjee is a clinical research expert with over 30 years of experience in drug development and pharmaceutical medicine. He has headed Medical Research departments in Pfizer India, Ranbaxy Laboratories, GVK Biosciences and Quintiles Asia.
He is the founder and was first President of the Indian Society for Clinical Research. Dr. Mukherjee has been involved in assignments across the pharmaceutical research and medical start-up domains as an independent consultant with assignments in pain, tropical disease, biologicals, vaccines, and phytopharmaceuticals.
In addition, Dr. Mukherjee is a member of research advisory boards of various private and public sector organisations. He is a recipient of the Indian Society for Clinical Research Lifetime Achievement Award for 'Exemplary Contributions in Building and Nurturing the Clinical Research Ecosystem in India' and Global Fellow in Medicines Development Award by the GMDP Academy, New York.
Welcome Onboard
 Dr. Swapnil Pathak
Dr. Swapnil Pathak
Associate Director - Cardiology
Medanta - Lucknow
Cardiologist with expertise in clinical and preventive cardiology, non-invasive diagnostic procedures, interventional procedures and cardiac rehabilitation.
 Dr. Ritesh Debroy
Dr. Ritesh Debroy
Senior Consultant - Uro-Anaesthesia
Medanta - Gurugram
Anaesthesiologist with expertise in administering anaesthesia to high-risk surgical cases, critical care management, difficult airway management, pain management in addition to central and arterial line placement in adult and paediatric patients.
 Dr. Sohet Gogia
Dr. Sohet Gogia
Consultant - Neurosurgery
Medanta - Gurugram
Neurosurgeon with expertise in neuro- oncology, functional neurosurgery including deep brain stimulation, epilepsy surgery, endoscopic neurosurgery and paediatric neurosurgery. He specialises in minimally invasive neurosurgery for both brain and spine.
 Dr. Navin Kumar
Dr. Navin Kumar
Associate Consultant - Gastroenterology
Medanta - Patna
Gastroenterologist with expertise in all therapeutic endoscopic procedures, ERCP and EUS-guided procedures, management of GI malignancies and IBS in addition to management of GI emergency.
 Dr. Shiv Prakash
Dr. Shiv Prakash
Associate Consultant - Rheumatology
Medanta - Patna
Rheumatologist with expertise in the treatment and management of rheumatoid arthritis, spondyloarthritis, inflammatory myositis, vasculitis, psoriatic arthritis, reactive arthritis, systemic sclerosis, gouty arthritis and other connective tissue disorders.







