THE EXCHANGE | Newsletter August 2018
Complex Glucose-6-Phosphate Dehydrogenase Case Treated at Medanta
A 36-year-old male, born to non-consanguineous parents presented with fever, chills and headache since seven days and hematuria since one day. Patient had been evaluated outside, found positive for Malaria (P. vivax) and administered anti-malarial drugs (Artesunate and Primaquine). Clinical condition of the patient did not improve. He did not respond to treatment and was referred to Medanta.
On presentation, patient was anemic (Hemoglobin- 5.8gm%) along with leukocytosis (Total Leucocyte Count {TLC}- 36.24X103/mm3), and was experiencing restlessness, fatigue, dyspnea, and air hunger. He was admitted to the Intensive Care Unit and initiated on IV fluids, IV antibiotics and other supportive measures.
Other biochemical investigations revealed deranged liver function tests - raised bilirubin and liver enzymes (Bilirubin- 8.8mg/dl; Direct 2.8mg/dl; SGOT-9615U/L; SGPT-2825U/L; gGT-223U/L ) and normal kidney function tests (Creatinine- 1.0mg/dl ). Patient's lactate dehydrogenase enzyme (LDH; 19504 U/L) was elevated, but both direct and indirect Coombs' tests were negative. Coagulation profile was normal which ruled out Disseminated Intravascular Coagulopathy (DIC).
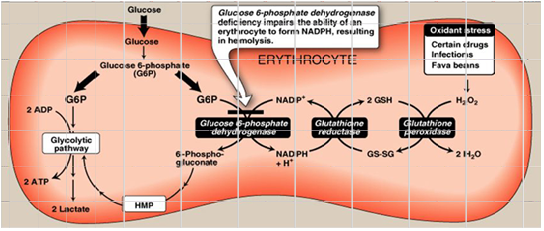
Pulse oximetry showed a recording of oxygen saturation between 75-80% in spite of proper oxygen support; Arterial Blood Gas (ABG) showed saturation above 90%. Co-oximetry resolved this mismatch and confirmed methemoglobinemia of 10.1U/g. Further testing revealed that the patient had insufficient quantities of G6PD enzyme activity on assay (0.1U/gHb; reference range: 4.6- 13.5 U/gHb). Provisional diagnosis of methemoglobinemia in G6PD deficient state - class II (as per WHO classification) was made and initially patient was put on high-flow nasal oxygen therapy. High Performance Liquid Chromatograpgy (HPLC) revealed no haemoglobinopathies. Severe hemolysis in the patient was inferred due to oxidative stress caused by infection itself or anti-malarial drugs (administered outside) or both. Hemolysis was aggravated due to underlying G6PD deficiency.
This led to a therapeutic dilemma for the treating team as the primary treatment for such critical patients with methemoglobinemia is intravenous Methylene Blue (MB). However MB is contraindicated in patients with G6PD deficiency as it increases hemolysis, further deteriorating the condition of the patient. Ascorbic acid, which is also used in treatment of methemoglobinemia is again considered a risk factor for haemolysis in G6PD deficient patients.
For the first 48 hours after admission, patient was maintained on medical management and non-invasive ventilation {Biphasic Positive Airway Pressure (BiPAP) system} only. However, there was worsening of methemoglobinemia (12.5U/g), and the patient showed signs of ongoing hemolysis on peripheral smear. In this situation, the primary treating physician and transfusion medicine specialist decided and planned therapeutic Red Cell Exchange (RCE) over methylene blue.
Automated exchange procedure was performed via hemodialysis-type double-lumen 16F catheter inserted in left femoral vein for unhindered blood flow. Procedure was performed on apheresis machine Com.Tec (Fresenius Kabi, Germany) using the standard PL1 kit (Fresenius Kabi, Germany). The machine has in-built software program for performing Red Blood Cell (RBC) exchange (primarily for sickle cell disease).
The patient underwent two RCE procedures on consecutive days. First procedure resulted in improvement in both clinical and laboratory paramters; methemoglobiemia decreased from 12.5U/g to 8.1U/g and air hunger decreased. To capitalise on the improvement after the first exchange, a second procedure, in a bid to wean the patient off the assisted ventilation, was performed. Following the second procedure, oxygen saturation further improved; 85-90% to 90-95% after the first, and to 95-100% after the second exchange procedure. Methemoglobinemia reduced to 0.1U/g.
Patient's vitals including pulse rate, blood pressure, oxygen saturation and respiratory rate were monitored before, during and after the procedure. Continuous intravenous calcium gluconate 10% (20ml in 80ml normal saline) infusion at the rate of 60ml/ hour was given to the patient during the procedures to prevent citrate effect. The two procedures lasted for mean 79 minutes and were completely uneventful.
During the hospital stay, 7 units RBC, 4 units RDPC and 1 unit Single Dose Platelet Concentrate (SDPC) were transfused to the patient besides 10 units RBC utilized in RCE procedures. The patient responded well to RCE and other supportive treatment and was shifted to room on day-10 with improved LFT (Bilirubin-4.8 to 1.8 mg%, SGOT- 6560 to 86 U/L, and SGPT- 2483 to 228 U/L), increased platelet count (28,000 to 338,000/µL), no hematuria and maintenance of oxygen saturation on room air. The patient was discharged on day-12. Patient is off medication and continues to do well.
(With inputs from Dr. Sushila Kataria, Dr. Aseem Tiwari and Dr. Vaibhav K Gupta)
Teaching Kitchen
A unique initiative by Medanta to help caregivers better respond to needs of their loved ones, the Teaching Kitchen is a healthy cooking workshop run by our dieticians and chef.
Since healthy food is vital to a patient's recovery and their continued well-being, this workshop trains caregivers in preparing delicious, healthy meals. The chef also shares patient-friendly recipes which can easily be prepared at home on vce the patient is discharged from the hospital.


Our Unique Critical Patient Monitoring and Recovery Technology
Medanta embraces technology eagerly. Early adopters of cutting-edge inventions, we are unique and trendsetting in much of what we do. A recent aspect of this core value is our collaboration with the well known US-based medical technology firm, Masimo Corporation (www.masimo.com) to introduce a unique critical patient monitoring and recovery technology. Only Medanta offers this in South Asia.
It is an established fact that calibrated physical effort led movement by patients has a significant role to play in recovery. Called Radius-7, this wearable, tether-less Pulse

CO-Oximeter works in conjunction with a bedside monitor to provide continuous non-invasive monitoring, while allowing patients freedom of movement. On a constant, dynamic, real-time basis, this wearable tool helps ensure patient stability, while accelerating recovery. The technology allows supplemental remote monitoring and clinical notification which enable monitoring of patient data remotely, as well as relaying alarm notifications to clinicians. The technology significantly reduces false alarms and increases true alarm detection, allowing clinicians to focus on the patients and alarms that need attention. Created around the world's most accurate pulse-oximetry technology, the system has been proven to reduce false alarms by 95% and increase true alarms by 97%. This has created a global benchmark in Oxygen Saturation Monitoring.
Radius-7 is lightweight and can be attached to the arm, allowing extended untethered monitoring for a patient at all times. This also reduces the need for physical nursing assistance by transcending the need to manage bedside monitors. The device continuously and non-invasively monitors vital parameters. Data is then sent to a server which communicates with a central system stationed in the ward where clinicians/nurses view vital parameters of the patient. In the event of any variations, the assigned nurse receives a notification on the pager. This is backed-up by an escalation protocol if the primary nurse does not respond within a stipulated time.


Dr. Naresh Trehan
CMD, Medanta
Medanta has institutionalized the best possible patient recovery ecosystem benchmarked to global standards. Adoption of Radius-7 illustrates our deep commitment to patient-centric clinical excellence.
Engaging the Waiting Patient
While we do a lot to minimize waiting time for patients, the reality is patients do spend time waiting. And if you observe them while they do so, patients seem to be perfectly satisfied immersing themselves in social media on their mobile phones, reading a magazine, or simply doing nothing until their name is called. This time can be constructively utilized to provide patients clinical education or simply improve the overall patient experience.
Here are a few tips:
- Update patient information. Thoroughly update details such as patient's address, phone number and email address. Consider providing patients with a print out or tablet while they wait so that they can update their information. This information helps in reminding patients about follow ups, drive therapy adherence and convey critical information such as off days or change in appointment schedule.

- Provide educational handouts about the dangers of non-compliance. For example, consider providing inputs on what can happen if a patient with diabetes doesn't take his or her insulin. This engages patients while they wait and provides subtle and non-intrusive education that can drive positive behaviour change.
- Offer free wi-fi and consider providing individual or shared work stations with charging stations if space permits. Patients often compromise work for their appointments; helping them be productive can alleviate stress and show you value their time.
- Ask patients to complete a brief satisfaction survey or drop a card in a suggestion box. This is a great use of patients' time, but one must also be prepared to respond to feedback.






