THE EXCHANGE | Newsletter - Apr 2023
Medanta Gurugram Recognized as the Best Private Hospital in India for the Fourth Time in a Row
World’s Best Hospitals 2023 Survey by Newsweek
Testimony to the world-class healthcare the hospital provides, Medanta Gurugram, has ranked as the
Best Private Hospital in India for the fourth consecutive time in the annual global survey conducted by Newsweek in partnership with Statista Inc. Medanta is the only Indian private hospital to feature in the top 200 of the World’s Best Hospitals 2023 survey list.
Conducted across over 2,300 hospitals in 28 countries, the survey is based on recommendations from over 8 lakh doctors and medical experts, results from patient surveys and key medical performance indicators such as quality of treatment and hygiene measures.
“Being recognised as the best private hospital in India for four consecutive years by patients and the doctor community is a testimony to the standard of clinical care we deliver, world-class medical infrastructure and advanced treatment technology that we offer to our patients. We are honoured to receive this recognition from a reputed and independent platform like Newsweek, and will continue furthering our commitment to making world-class healthcare accessible to all.”
Dr. Naresh Trehan
Chairman and
Managing Director
Medanta

Infocus
Medanta Launches Women and Child Care Services in Gurugram
Welcomes Dr. Praveen Khilnani, Dr. Rajiv Uttam, Dr. T.J. Antony and
Dr. Preeti Rastogi

Bringing comprehensive, world-class women and child care services on a common platform, Medanta - Gurugram has launched the Institute of Women and Children. Led by
Dr. Praveen Khilnani, the Institute will be a center of excellence for neonatal and paediatric care, obstetrics and gynaecological disorders. Dr. Khilnani (Chairman) – will be supported by eminent paediatric critical care specialist Dr. Rajiv Uttam (Director and HoD – Paediatrics, Paediatric ICU and Paediatric Emergency), neonatology expert Dr. T.J. Antony (Director and HoD - Neonatology and Neonatal ICU), and high-risk obstetrics and gynaecology expert Dr. Preeti Rastogi (Director and HoD – Obstetrics and Gynaecology).
Women of all ages – right from the onset of puberty to pregnancy, menopause and beyond – will get round-the-clock access to comprehensive treatment backed by advanced technology, state-of-the-art infrastructure and facilities here. The Obstetrics and Gynaecology department, led by Dr. Preeti, will be equipped to provide complete obstetrics care, including high-risk pregnancies and painless childbirth, and treatment of all gynaecological conditions.
To ensure the well-being and address the health complications of children across all age groups (from birth till 18 years of age) the general Paediatrics, Paediatric Intensive Care and Paediatric Emergency department, led by Dr. Uttam, will provide dedicated services across all paediatric super specialties. The Neonatal Intensive Care Unit, led by Dr. Antony, will offer all the latest facilities required to treat even the most severely ill neonates. It will also provide developmental supportive care to newborn babies, such as day-night light cycling and facilities for kangaroo mother care. The world-class facility will also provide care for extremely small preterm babies weighing less than 1 kg.
The Level-3 paediatric and neonatal ICUs will be equipped with high-end supportive infrastructure, including echocardiography, ECMO (extracorporeal membrane oxygenation), therapeutic hypothermia, inhaled nitric oxide, total parenteral nutrition, double wall incubators, transport incubators, volume-targeted ventilation, high-frequency ventilation, and other ventilation techniques, such as non-invasive mechanical ventilation (NIMV), continuous positive airway pressure (CPAP) and heated humidified high-flow nasal cannula (HHHFNC). The paediatric and neonatal teams will be supported by paediatric super-specialists from all departments. The institute will also provide 24x7 paediatric emergency care, supported by paediatric transport services.
Medanta Accelerates Efforts for Mission TB Free India
Anchors Collaboration with Private Hospitals in Delhi-NCR to Scale Tuberculosis Screening

With an aim to galvanise private hospitals from across Delhi-NCR to contribute to the National Tuberculosis Elimination Programme (NTEP), and expand the impact of Mission TB Free India, Medanta – in association with The Union, under the guidance of Central TB Division, MoHFW – organised a multi-stakeholder event engaging private hospitals and state health officials. As part of the programme, deliberation was held with Apollo Medical College, Yashoda Super Specialty Hospital, Amrita Hospital and stakeholders from a number of other hospitals. They were encouraged to support the national initiative by adopting the ‘Active Case Finding’ model of TB detection that has been championed by Medanta over the years.
Towards the Pradhan Mantri TB Mukt Bharat Abhiyan, Deputy Director General of Central TB Division, MoHFW, Mr. Rajender P. Joshi, announced the private hospitals’ engagement programme in the presence of Dr. Naresh Trehan (Chairman and Managing Director, Medanta), Dr. Anand Jaiswal (Senior Director) and Dr. Bornali Datta (Director) from the Department of Respiratory and Sleep Medicine in Medanta - Gurugram. The event was also graced by Dr. Kuldeep Sachdeva (Regional
Director – SE Asia, International Union Against Tuberculosis and Lung Diseases).
The objective of this engagement programme is to encourage private hospitals to actively contribute to TB screening and assist the state in bridging the gap in TB care services. This will further strengthen the robust NTEP that works to detect TB in unscreened population pockets, and establish linkages between identified patients and government treatment services.
Using Medanta’s active case finding methodology, its community health workers and village-level grassroots health workers (ASHAs) regularly conduct door-to-door screenings to detect individuals at potential risk. For on-spot diagnosis, they use sputum analysis, digital chest X-ray and an artificial intelligence-based tool (Qure.AI) followed by a highly-advanced confirmatory molecular-diagnostic test (GeneXpert). All these diagnostic facilities are available in dedicated mobile vans that travel to villages as part of the Mission. Confirmed TB cases are referred to government hospitals for initiation of DOTS (Directly Observed Therapy Short) course therapy. The block-level screenings, being done as cluster randomized control trials, have defined an effective model for finding active cases. The initial results have been promising as the team could diagnose 200 patients from four blocks of Karnal (Haryana) in just five months.
Dr. Naresh Trehan (Chairman and Managing Director, Medanta) said, “Timely screening, detection and treatment play a crucial role in the prevention and management of tuberculosis. Currently, a vast majority of patients go undetected and untreated in India, significantly increasing the disease burden. The private hospital sector can play an important role in the prevention and treatment of TB by taking on a larger, more active role in screening. We are delighted to share our learnings with other private hospitals and scale the TB-Free initiative through widespread adoption of the cost-effective screening model developed by Medanta.”
Medanta@Work
Thoracic Endovascular Aortic Repair (TEVAR) in Traumatic Thoracic Aortic Transection
The development of thoracic endovascular aortic repair (TEVAR) has allowed a minimally invasive approach for management of an array of thoracic aortic pathologies. Initially utilised in the treatment of aortic aneurysmal disease, indications of TEVAR have expanded to include treatment of Type B aortic dissection with malperfusion or rupture, traumatic aortic transection, and penetrating aortic ulcer (PAU). Although there are no randomised controlled trials directly comparing TEVAR to open surgery, numerous studies suggest that TEVAR is associated with decreased morbidity compared with open repair. Benefits of the endovascular approach include avoidance of thoracotomy or sternotomy incision, avoidance of aortic cross-clamping, decreased blood loss and decreased end-organ ischemia.
Case Study
A 49-year-old hypertensive, non-diabetic male patient presented in the Emergency of Medanta-Patna one week after a road traffic accident with persistent pain on the left side of his chest. He had a fractured femur for which intramedullary (IM) nailing was done at another centre followed by strapping for multiple rib fractures. At the same centre, he had undergone an electrocardiogram (ECG), which was normal. His contrast-enhanced CT (CECT) scan of the chest showed posterior mediastinal haematoma along with chest wall haematoma. Hence, he was referred for further evaluation and management of haemothorax to Medanta - Patna.
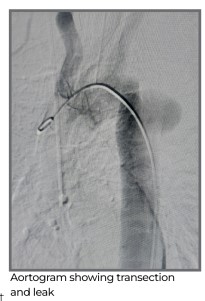
Post evaluation, a CT aortogram was done that showed aortic transection at the level of isthmus of aorta, which is a usual site for high-velocity traumatic injury in the aorta due to its anatomical location. In high-velocity road traffic accidents, rapid deceleration of upper body due to impact
of encountered object(s) causes shearing stress on the aortic wall. The CT aortogram showed contained rupture of descending thoracic aorta at the level of isthmus. His serum creatinine was 1.5 mg/dl and ultrasound whole abdomen was normal. Echocardiography (ECHO) showed normal LV function with no pericardial collection.
After the diagnosis of aortic transection, the patient was planned for urgent intervention. After discussing the risks and benefits of open surgery and endovascular therapies, the patient consented for endovascular procedure.
Patient was evaluated in the intensive care unit (ICU) and was taken up for TEVAR under general anaesthesia. Vascular access was achieved through right femoral artery. Pigtail catheter was used to delineate and measure the rupture extent and stent size. This was followed by deployment of stent over 0.035 system over stiff amplaz wire.
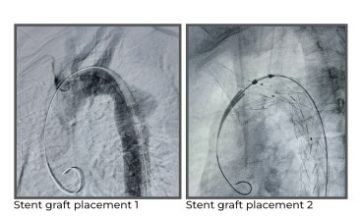
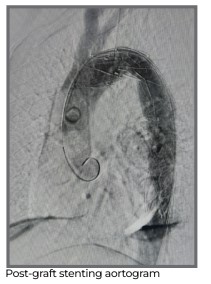
Deployment of stent was uneventful. Post deployment testing showed left subsclavian artery covered. Right femoral artery was repaired and distal pulses were palpable.
Post procedure, the patient was shifted to the ICU. His left upper limb remained normal.
Patient was observed in the ICU for 24 hours and kept on relevant medicines. On Day 2, patient was shifted to the ward and discharged from the hospital on Day 3 of the procedure.
On second followup after one month, the patient was doing well.
Dr. Sanjay Kumar
Director – CTVS, Cardiac Surgery
Heart Institute
Medanta – Patna
Dr. Rajeev Ranjan
Director – CTVS ICU and Anaesthesia
Medanta – Patna
Mega Prosthesis in a Case of Resistant Non-Union Distal Humerus Fracture
A fracture is considered as resistant non-union when the affected bone cannot be joined despite multiple failed surgical approaches. Resistant non-union fractures of distal humerus are managed by total elbow arthroplasty. There are case reports wherein mega prosthetic replacement has been done with good results. We report a case of old, resistant non-union of distal humerus with a huge clinical deformity and failed implant in situ. The procedure was challenging due to anatomical distortion, bone gap and risk of damage to the neurovascular structures.
Case Study
A 35-year-old male patient with a body mass index (BMI) of 48.5 kg/m2 presented at Medanta - Lucknow with non-union of distal humerus fracture. Six years ago, he had sustained an injury on the left arm in a road traffic accident resulting in comminuted fracture of distal end of the humerus. At another centre, he had already undergone open reduction and internal fixation that failed to unite. A year on, he underwent another surgery for implant removal and re-fixation of the fracture with bone grafting, which also failed. The distal humerus fracture progressed to non-union with severe deformity and stiffness of the elbow with a jog of movement of 10 degrees. He came to Medanta for correction of the elbow deformity and to gain reasonable elbow and hand function.
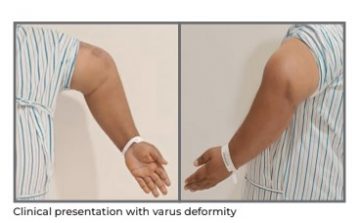
On evaluation, it was found that there was a significant mass of about 9-10cm in diameter on
the lateral aspect of the elbow and there were no signs of nerve involvement. However, hand function was affected by stiffness in wrist and fingers. Plain radiographs showed failed implant in situ with hypertrophic non-union of the supracondylar fracture along with deformity at the distal humerus due to mal-united distal humeral fracture. In view of grossly distorted anatomy of the distal humerus, bone gap at the non-united fracture, severe elbow deformity and stiffness, a mega prosthetic replacement of the left elbow
was planned.

Under general anesthesia, elbow was approached posteriorly and the fracture site was exposed. A gross hypertrophic bone formation on the antero-lateral aspect of the humerus was found entrapping the neurovascular structures. Due to fibrosis, the anatomical planes were distorted. Controlled dissection was performed to isolate the neurovascular structures, especially the radial nerve. The distal humeral condylar fragments had been destroyed with arthritic changes in the joint. Salvage procedure for the elbow joint would have been a futile exercise because of loss of joint cartilage.
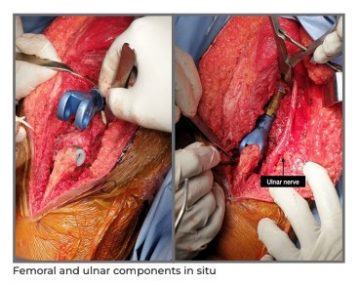
Implant and the distal humeral bone fragments were excised. Proximal ulnar preparation was done and appropriate implant size was determined. Cemented titanium prosthesis was used for the reconstruction of elbow. Intra operatively, correction of the elbow deformity was successfully achieved with range of movement (ROM) of 5 to 130 degrees and stable elbow joint. The ROM was achieved despite morbid obesity. Closure was done over a drain.
Passive ROM was initiated after 24 hours of the surgery and the drain was removed after 36 hours with less than 100ml output volume. The patient was discharged on Day 3 of the surgery. During follow up on Day 7, there was 90 degrees of active elbow flexion with no soakage.

On his four-week follow up, the patient was able to perform 100 degrees of shoulder abduction with 0 to 110 degrees active ROM at the elbow.
The patient continues to be on follow up and is progressing well.
Dr. Saif N Shah
Director - Orthopaedics
Institute Of Musculoskeletal Disorders
and Orthopaedics
Medanta – Lucknow
Dr. Hatif Qamar Siddiqui
Consultant - Orthopaedics
Institute Of Musculoskeletal Disorders
and Orthopaedics
Medanta – Lucknow
TechByte
Prostatic Artery Embolisation
Novel Technique for Prostate Treatment
Symptomatic benign prostatic hyperplasia (BPH) is a common condition in the aging population that results in troubling symptoms in the lower urinary tract impacting quality of life. Patients are often treated with medication and offered surgery for persistent symptoms. Transurethral resection of the prostate is considered the traditional standard of care, but several minimally invasive surgical treatments are also offered.
Prostatic artery embolisation (PAE) is emerging as an effective treatment option with few reported adverse effects, minimal blood loss, and infrequent overnight hospitalisation. The procedure is offered to patients with moderate to severe lower urinary tract symptoms and depressed urinary flow due to bladder outlet obstruction. Proper patient selection and meticulous embolisation are critical to optimise results.
Some indications for PAE may include:
- Moderate-to-severe urinary symptoms: Men with BPH may experience symptoms such as frequent urination, difficulty starting urination, weak urine flow, and incomplete emptying of the bladder. PAE may be recommended for those who have not responded well to medication or wish to avoid traditional surgical treatments.
- Prostate size: PAE is typically recommended for men with prostates that are larger than 30 to 40
grams. This is because larger prostates are more difficult to treat with medication and may require surgery. - Age and overall health: PAE may be recommended for older men who may not be good candidates for traditional surgical treatments due to their age or overall health.
- Desire to avoid surgery: Some men may prefer to avoid surgery due to the potential risks and complications associated with traditional surgical treatments.
- Medication intolerance: Some men may not be able to tolerate the side effects of medication used to treat BPH. PAE may be a good alternative for such patients.
It is important to note that PAE is not appropriate for all men with BPH. Men who have prostate cancer, active prostate infection, or severe urinary blockage may not be good candidates for PAE. It is important to discuss all treatment options to determine the best course of treatment for individual cases.
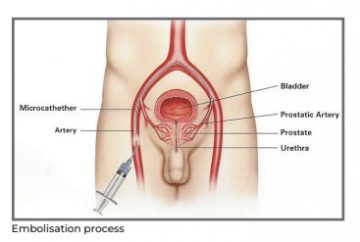
Case Study
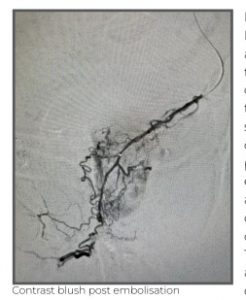
A 65-year-old male with a history of benign prostatic hyperplasia (BPH), presented at Medanta – Gurugram with lower urinary tract symptoms (LUTS) that had not responded to medication. His International Prostate Symptom Score (IPSS) was 28, indicating severe symptoms. Hence, he was advised for prostatic artery embolisation (PAE).

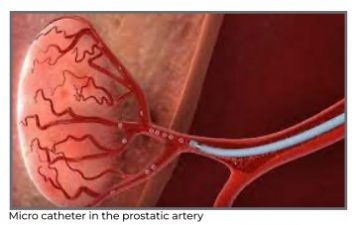
The patient underwent the procedure under local anaesthesia. A catheter was inserted into the femoral artery and navigated to the prostatic artery using X-ray guidance. Embolic agents were then injected to block blood flow to the prostate gland. The procedure went well with good clinical outcomes and the patient reported significant improvement in his LUTS within a few weeks after the procedure. His IPSS decreased to 10, indicating mild symptoms. He was able to urinate more easily, and had less urinary frequency and urgency.
Patient had no major complications from the procedure and was discharged on the same day. He returned for follow-up appointments after 3, 6, and 12 months post procedure, and continued to report improvement in his symptoms. His IPSS remained stable at 10, and he did not require additional treatment for BPH.
PAE is emerging as an effective minimally invasive treatment for lower urinary tract symptoms caused by BPH. It is safe, effective and has several benefits compared to traditional surgical treatments for BPH, including:
- Minimally invasive: PAE is performed through a small incision in the groin, and does not require general anaesthesia or major surgery. This means that patients typically experience less pain, bleeding, and scarring compared to traditional surgical treatments.
- Short recovery time: Most patients are able to return home on the same day or the day after the procedure, and can resume normal activities within a few days. Traditional surgical treatments, on the other hand, may require several weeks of recovery time.
- Lower risk of complications: PAE has a lower risk of complications compared to traditional surgical treatments, such as bleeding, infection, and sexual dysfunction. The risk of urinary incontinence, a common side effect of surgery, is also lower with PAE.
- Effective: Studies have shown that PAE is effective in reducing the symptoms of BPH, such as urinary frequency, urgency, and difficulty in urination. Many patients experience significant improvement in their symptoms within a few weeks after the procedure.
- Repeatable: PAE can be repeated if necessary, unlike surgical treatments that remove part of the
prostate gland. This means that if the symptoms of BPH return, another PAE can be performed to
provide additional relief.
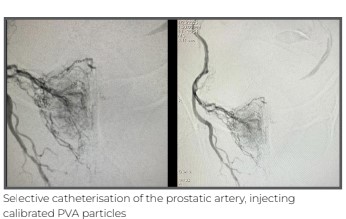
In conclusion, PAE provides an effective treatment option to relieve symptoms caused by prostate enlargement and bladder outlet obstruction. This offers an additional option in the spectrum of treatments for BPH that may be appropriate for select groups of men, including those with large prostates, or surgical comorbidities, those who cannot stop taking anticoagulation therapy for surgery, those with a strong desire to preserve sexual function, and those looking to treat concurrent lower urinary tract symptoms and haematuria with a single procedure.
Dr. Tarun Grover
Director - Peripheral Vascular and
Endovascular Sciences
Medanta – Gurugram
Spotlight
Medanta Gurugram Strengthens Awareness on Colorectal Cancer
To strengthen the fight against colorectal cancer by creating awareness around prevention, early detection, timely intervention and treatment, Medanta - Gurugram celebrated Colorectal Cancer Awareness Month. Lit in blue lights – the official colon cancer colour – symbolising solidarity in the fight against the disease, the hospital set up an innovative colon-shaped tunnel at the entrance. Each visitor at Medanta passed through this walk-through educational exhibit that highlighted the symptoms and stages of colorectal cancer. Offering an immersive, visually stimulating experience, the tunnel was a unique medium through which medically relevant information was disseminated, allowing for high recall value. Several community awareness programmes were organised in the form of health talks by leading gastroenterologists and gastro surgeons, free consultations with specialists and subsidised preventive screening programmes.

Welcome Onboard

Dr. Vibhu Priyadarshi
Director - Internal Medicine
Medanta - Patna Internal Medicine expert with over 40 years of experience in treating infectious diseases
(acute and chronic), haematological diseases, rheumatic diseases and ailments of the immune system. He also specialises in treating cardiac diseases, hepatobiliary diseases, pulmonary diseases (asthma, tuberculosis, COPD, interstitial lung disease) in addition to metabolic disorders such as diabetes, thyroid illness and gouty
arthropathy.

Dr. Prarthana Saxena
Associate Director - Neurosurgery
Medanta - Lucknow A highly skilled neurosurgeon with over a decade’s experience and expertise in endoscopic neurosurgery. She specialises in endoscopic skull base surgery, minimally invasive spine surgery (MISS), paediatric neurosurgery, neuro-onco surgery, carotid endarterectomy, complex aneurysm clipping and innovative endoscopic treatment for intraventricular haemorrhage, brain stroke and craniocervical junction abnormalities.

Dr. Arvind Kinger
Senior Consultant - ENT
Medanta - Indore
ENT specialist with expertise in endoscopic nasal surgery, rhinoplasty, endoscopic ear surgery, skull base surgeries in addition to thyroid and parotid surgery.

Dr. Mona Kulpati
Senior Consultant - Paediatrics
Medanta – Gurugram
Paediatrician with expertise in child nutrition, newborn care and growth monitoring, immunisation and developmental assessment. She also specialises in treating common childhood infections, allergies, asthma, GI conditions, skin disorders in addition to lifestyle and behavioural concerns.

Dr. Swati Kalra
Senior Consultant - Paediatrics
Medanta - Gurugram
Paediatrician with expertise in child nutrition, newborn care and treating childhood diseases with special interest in developmental paediatrics.

Dr. Mukul Pandey
Consultant - Paediatrics, PICU
and Paediatric ER
Medanta - Gurugram
Paediatrician with expertise in paediatric critical care and emergencies.

Dr. Sneha Bhatia
Consultant - Neonatology and NICU
Medanta - Gurugram
Naeonatologist with expertise in managing Level 3 NICU, including ventilation, complex neonatal procedures, care of extremely low birth weight babies and high-risk developmental follow-up of newborns discharged from NICU.

Dr. Karan Ahluwalia
Consultant - Paediatrics, PICU
and Paediatric ER
Medanta - Gurugram
Paediatrician with expertise in managing multiorgan dysfunction syndrome, acute respiratory distress syndrome, renal replacement therapy, in addition to non-invasive cardiac, respiratory and neurological monitoring.

Dr. Nilesh Srivastav
Consultant - CTVS
Medanta - Patna
Cardiothoracic surgeon with expertise in heart failure surgical therapies (heart and lung transplant, LVAD, RVAD) and complex cardiac surgical procedures (aortic and redo surgeries).

Dr. Anurag Goyal
Associate Consultant - Cardiac Surgery
Medanta - Gurugram
Cardiac surgeon with expertise in performing all routine adult cardiac, thoracic and vascular surgeries.

Dr. Pankaj Kumar
Associate Consultant – Neurosurgery
Medanta – Lucknow
Neurosurgeon with expertise in treating neurological disorders and spine diseases. He also specialises in endoscopic neurosurgery and treatment of traumatic brain injuries.

Dr. Prashant Choudhary
Associate Consultant – Paediatrics,
PICU and Paediatric ER
Medanta - Gurugram
Paediatrician with expertise in paediatric critical care and treating children with infectious diseases and emergencies.

Dr. Esha Gupta
Associate Consultant - Obstetrics
and Gynaecology
Medanta - Gurugram
Gynaecologist with expertise in high- risk pregnancy and delivery, complex gynaecological surgeries in addition to gynaecological oncology, laparoscopic and hysteroscopic surgeries.

Dr. Ashish Kumar Garg
Associate Consultant - Interventional Cardiology
Medanta - Gurugram
Interventional cardiologist with expertise in coronary angiography, angioplasty and stenting.






