Inflammatory Bowel Disease (IBD): Why it can get worse and what to do if it does?
Inflammatory Bowel Disease is a term used to categorise diseases that are caused due to an inflammation that disrupts bowel movements. There has been a steady rise in reports of IBD in Indians of late due to increased urbanisation, changes in lifestyle and diet, and environmental pollution, and studies have shown that people living in developing countries are more prone to IBD because of various factors such as hygiene and sanitation, lifestyle choices, and environmental factors.
What are the types of Inflammatory Bowel Disease?
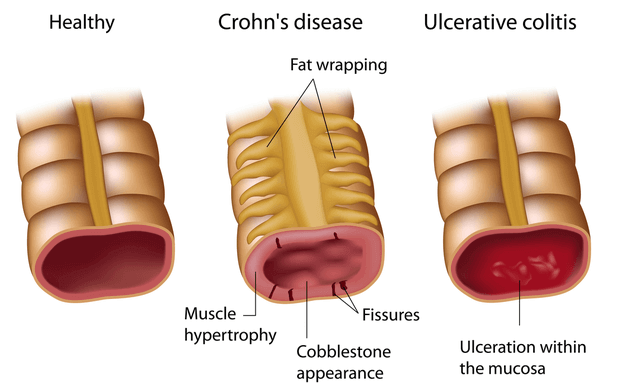
There are two types of IBD, namely - Ulcerative Colitis, and Crohn's's Disease. Both are accompanied by Diarrhea, pain in the abdomen, sudden weight loss, and fatigue.
- Ulcerative Colitis typically affects the inner lining of your colon, which is the large intestine, and the rectum, and can have long-lasting effects.
- While Crohn’s Disease is characterised by inflammation along your digestive tract and is prone to spread to other parts of your tissues.
So, here’s what you need to know about IBD:
What causes IBD?
The most well-known cause of Inflammatory Bowel Disease is a malfunction in your immune system. When your immune system tries to fight off harmful virus or bacteria, it may often lead to an attack in the cells of your digestive tract. IBD can also be caused due to hereditary factors. Earlier, it was believed that poor diet and stress could cause IBD, but doctors have concluded that it only aggravates the condition.
What factors increase the risk of IBD?

A number of factors can contribute to the development of Inflammatory Bowel Diseases. The most common factors are:
- Age: Most people are diagnosed with IBD before the age of 30. For others, they don’t develop it until 50 or 60 years of age
- Family history: If your family has had a history of IBD, you are more likely to be more susceptible than others
- Medicines: Some non-steroidal, anti-inflammatory medicines can also aggravate IBD, if already present, or create risks of developing one
- Cigarette smoking: Tobacco intake is perhaps the most controllable risk factor. Avoid smoking to be on the safer side
- Environment and Diet: Environmental factors and dietary choices can increase your risk of developing IBD. If your diet includes a high content of refined foods or fat, you will be more susceptible to the disease
What IBD Symptoms should you look out for?
Signs and symptoms of IBD vary from mild to severe, depending on which part of the tract it is affecting. Typical symptoms include:
- Blood in the stool
- Diarrhoea
- Abdominal Pain and severe cramps
- Iron deficiency due to blood loss
- Frequent urge to defecate
- Fever and weight loss
What makes IBD worse?
Although there is no particular reason to pinpoint as to what can make IBD worse for you, here’s a collective list of probable causes that can make it worse:
- Food: Excessive use of caffeine, alcohol, smoking, dairy products, fizzy drinks, high-fibre foods, and oily or spicy food can directly affect your IBD, be it Ulcerative Colitis, or Crohn's Disease
- Skipping Medicines: If you’re already diagnosed with IBD, it is advisable to maintain a regular schedule of your prescribed medicines
- Excessive stress: Stress can cause inflammation and make it even harder for you to deal with IBD
How can IBD be diagnosed and treated?

To confirm if you have IBD or not, your doctor will perform a few tests on you. They might be:
- Colonoscopy: A procedure that involves inserting a flexible tube of about half an inch into your rectum, to scan the tract and diagnose what’s wrong
- Blood tests: That will help detect infection and Anemia
- Sigmoidoscopy: While the Colonoscopy will view your entire colon, the Sigmoidoscopy will only view the lower part of your colon for visible signs
Once diagnosed, based on your test results, the doctor will suggest changes and medications that ease any pain and discomfort. Your doctor may suggest:
- Anti-inflammatory medicines, which are the first steps to treating IBD
- Immune System Suppressors, that work in more than one way to suppress the chemicals released by your immune system
- Antibiotics, and other supplements that help relieve the pain caused by inflammation
What can you do to ease IBD pain?
Your doctor might suggest dietary and lifestyle changes post-treatment. So here are a few simple things you can do:
- Keep a food journal: Track everything you eat and how you have been affected by it. This will help you understand what food items to avoid or consume in the long run
- Manage your stress better: Stress can be a major contributing factor to aggravating IBD. Find better ways to manage your stress, by using meditation techniques to control your breathing and heart rate
- Review your medicine with your doctor at regular intervals: It’s imperative to discuss the progress of your treatment with your doctor. If something isn’t working out for you, share that information and find out alternatives to the treatment
- Don’t smoke: Tobacco is an aggravator of IBD, so it’s best to quit smoking right after diagnosis
There are several other ways to cope with Inflammatory Bowel Diseases. Reach out for help, talk, join support groups, be aware of your body and mind, and consult your doctor whenever you need him.






