What You Need To Know About Getting A Colonoscopy

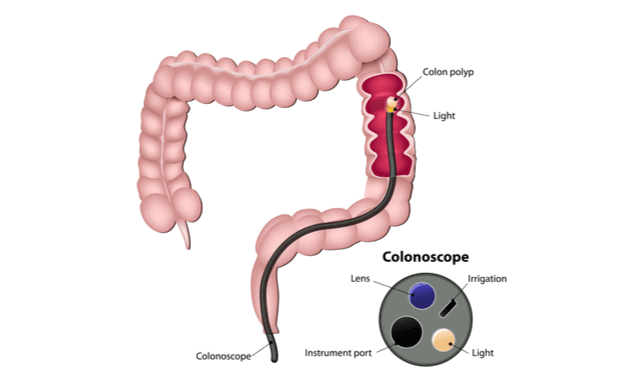
Colonoscopy is a procedure employed to check the lining of your colon and gauge any problems in your large intestine (colon) and rectum. It is one of the most accurate tests for detecting abdominal and rectal cancers, and is frequently used as a screening tool to test for gastrointestinal diseases including Polyps (abnormal growths in the lining of your colon).
When Will You Need Colonoscopy
Your doctor may suggest a colonoscopy if you begin to display symptoms like:
- Painful bowel movements or a feeling that you haven’t completely emptied your bowels
- Diarrhoea, constipation, or change in bowel habits
- Bright red or very dark blood in your stools
- Thinner or narrower stools than usual
- Sudden weight loss
- Pain in the abdomen with frequent cramps and bloating
How Is a Colonoscopy Done?

A Colonoscopy usually involves the insertion of a flexible tube into your rectal cavity, called a Colonoscope. This tube is half an inch in diameter and around 5 ft in length. The end that goes into your body has a tiny camera and light attached to it, which allows your doctor to see the inside of your system.
For the test, you will be given medication which will relax you and make you a little drowsy. You will be asked to lie down on your left side and then gradually, the tube will be inserted. The doctor will navigate the tube till it reaches your big intestine. You might be asked to move a little sometimes, to adjust the colonoscope.
In certain cases, if the doctor notices any abnormality, tiny pieces of your tissue are taken using a 'snare', for further testing. This is called a biopsy. The test will take around 30 minutes and once done, the doctor will gradually take the tube out, carefully examining the abdominal lining.
You can rest a little after the procedure and then leave though you will be advised not to drive or exert yourself soon after the test.
Precautions Before a Colonoscopy
A colonoscopy poses a few risks, such as the development of tears in the lining of your colon or rectal wall, allergic reactions to the sedatives used during the procedure and bleeding in the area where the tissue sample was taken.
Here are a few precautions you can take before you undergo a colonoscopy:
- Pre-Colonoscopy Diet: You will be advised to avoid solid foods, coloured drinks because it can mask the lining of your colon and interfere with the examination. You will be instructed to consume plenty of clear liquid and even tea or coffee but without milk. The aim is to ensure your colon is completely cleared .
- Use an enema kit: It helps soothe constipation and relieve bowels. Take as advised by your doctor, before a colonoscopy. Enema kits are available in most medical shops
- Have a laxative: Take a tablet or liquid laxative the night before, or as advised by your doctor to clear your colon
- Review your existing medication: Make it a point to inform your doctor of any active prescriptions to avoid any unintended drug reactions, especially in case of drug allergies, diabetes, any heart condition and such.
Questions to Ask Your Doctor After a Colonoscopy

You can speak to your right after the procedure, for some do's and don'ts for the next few days. They will mostly be either Dietary (what not to eat to aggravate discomfort) and Medications (which medicines not to take for some time, based on your medical history).
It is common to find some bleeding after a colonoscopy. Alert your physician if you experience any post-procedure discomforts.
How Often Should You Get a Colonoscopy?
After the age of 40 years, it is advisable to get a Colonoscopy every 10 years. However if yours first test yielded polyps, you should get it done every 5 to 10 years. Based on your results, you will be asked to do another procedure, or follow a rigorous surveillance routine as prescribed.
Contact your physician if you experience heavy bleeding for a long period of time, or get chills, fever, or severe abdominal cramps.