THE EXCHANGE | Newsletter - September 2023
Medanta Launches e-ICU Services for Enhanced
Critical Care Access
When it comes to treating a diversified patient population, the need for professionals with a multidisciplinary background has been ever-increasing, especially in closed ICU systems. Every new patient in the ICU poses a different challenge, which requires looking at the particular case from multiple perspectives before arriving at a diagnosis. To meet the current demand for modern critical care and to make sure that patient care is not compromised, Medanta has launched India’s most unique and unmatched e-ICU services as the Medanta e-ICU project in association with GE HealthCare, with a vision to nurture 'super-speciality based critical care practices'. This revolutionary project aims to leverage e-ICU technology to bridge the existing gap between super-specialised critical care expertise and underserved communities through timely interventions and reduced response times via 24x7 Medanta e-ICU Command Centre.
The Medanta e-ICU Command Centre at Medanta - Lucknow was inaugurated by the Hon’ble Chief Minister of Uttar Pradesh, Shri Yogi Adityanath.

This medical technology-driven platform provides near-real time updates for remote patient monitoring and early interventions, at all times. As a result, the decision-making ability of an ICU is enhanced and can bring extraordinary results in clinical outcomes.
The Medanta e-ICU Command Centre offers a solution by facilitating direct machine-to-machine integration, leading to enhanced efficiency, improved patient care, reduced costs, and an overall better experience for both patients and clinical teams.
The Inner Workings of Medanta e-ICU
The Medanta e-ICU infrastructure has been optimised to offer the most efficient and effective patient care. Here’s a step-by-step breakdown of our e-ICU process:



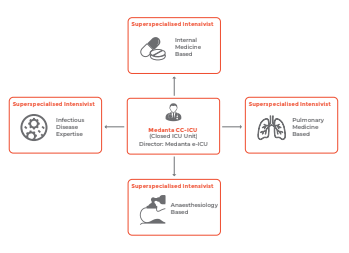
Composition of Medanta e-ICU Team
Medanta e-ICU has a team of highly qualified intensivists with diverse backgrounds, committed to delivering comprehensive care without delays.
A cohort of 4 consultant-level ICU specialists works as one unit in the command centre and are assigned duties on a rotation basis.
Reaching Patients in all Corners
At Medanta, our objective is to make our e-ICU services and world-class experts available to our patients wherever they are. To that end, we have created a strong supportive infrastructure that includes Medanta’s ‘Flying Doctors India’, which is equipped with a fleet of 7 aircrafts, each with a dedicated team of specially trained doctors, nurses, pilots and support staff to help evacuate patients from even the most remote areas. It provides ailment-based specialists and air-worthy equipment, including neonatal ventilators and intra-aortic balloon pump (IABPs), all of which are available 24x7.


Medanta@Work
Advancing Fight Against Non-Seminomatous Germ Cell Tumours with Robotic Retroperitoneal Lymph Node Dissection
Non-seminomatous germ cell tumours (NSGCTs) are aggressive malignancies that commonly affect young men. Radical orchiectomy is the standard treatment for localised disease followed by adjuvant chemotherapy for high-risk cases, and surveillance for low-risk cases.
Following Bleomycin, Etoposide and Cisplatin (BEP) chemotherapy, only 6%-10% of residual masses contain active cancer, 50% of which have post-pubertal teratoma and 40% have necrotic-fibrotic tissue only. Resection is mandatory in all patients with a residual mass greater than 1cm in greatest diameter at cross-sectional imaging.
Retroperitoneal lymph node dissection (RPLND) is a surgical procedure that is indicated for patients with NSGCTs with residual masses or positive lymph nodes even after chemotherapy, or for those with stage-II or -III disease at presentation. RPLND is associated with significant morbidity, including retrograde ejaculation, erectile dysfunction, and vascular injuries.
Robot-assisted RPLND (RA-RPLND) is a minimally invasive surgical technique that has gained popularity in recent years. This approach allows for improved visualisation and access to the retroperitoneal lymph nodes, reduced blood loss, and shorter hospital stay compared to open surgery. Additionally, RA-RPLND has been associated with lower rate of postoperative complications, such as wound infections and ileus. The use of the Da Vinci Surgical System has made RA-RPLND a feasible option for patients with NSGCTs with high success rates and low morbidity.
In this case study, we present a patient with NSGCT who underwent successful RA-RPLND along with right pelvic lymph node dissection using a common port position with no postoperative complications.
Case Study
A 23-year-old male presented to Medanta - Gurugram with a diagnosis of NSGCT of the right testis. He had undergone right high inguinal orchidectomy in November 2022, and histopathology revealed embryonal cell carcinoma. He received 4 cycles of chemotherapy with the BEP regimen in his home country, with the last cycle completed in February 2023. The patient's post-chemotherapy Alpha-fetoprotein (AFP) was 3.82ng/mL, and human chorionic gonadotropin (HCG) was less than 0.5mIU/mL. The patient had no comorbidities at the time of presentation. His haemoglobin was 12.9g/dl and serum creatinine was 1.3mg/dl. Positron emission tomography - computed tomography (PET-CT) scan was done and was compared to the PET-CT scan done in the previous year. It was suggestive of partial response with reduction in size, number and Fluorodeoxyglucose (FDG) uptake of the metastatic lymph nodes in aortocaval, common and external iliac regions. Present findings included enlarged external iliac lymph node (1.5cmx1cm), common iliac lymph node (1cmx1cm) and a nodal mass (3cmx4cm) in the interaortocaval region just below the renal vessels. There was an absence of FDG avid disease in the rest of the regions surveyed. The patient was planned for Robotic RPLND with right pelvic lymph node dissection using a common port position.
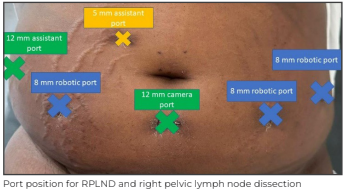
Intraoperatively, the patient was first placed in a low lithotomy position. Docking of Da Vinci Si robot was done in lithotomy position for the right pelvic lymph node dissection first. Six ports, including three 8mm, two 12mm, and one 5mm port were inserted keeping in mind the use of common ports for RPLND part of the procedure with camera port placed below the umblicus. There was an intense pelvic desmoplastic reaction seen along the nodes due to chemotherapy. Right pelvic lymph node dissection was done. The right gonadal vein was identified and dissected distally up to the silk suture ligature at the stump of the spermatic cord. The right external, internal, and common iliac group of lymph nodes were dissected and removed.
The robot was then redocked from above the left shoulder using the same ports. Only one extra assistant port was needed for RPLND, which was placed in right iliac fossa. Bilateral common iliac vessels, aortic bifurcation and the right ureter were identified. An incision was made over posterior peritoneum at the root of mesentry.
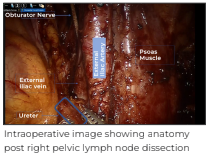
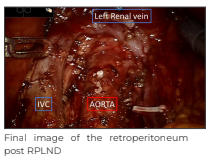
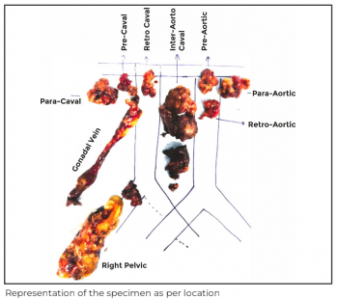
Dissection was continued in cephalad direction in continuation with proximal extent of right common iliac node dissection. Great vessels were identified and cut along the edge of the peritoneum; overlying small bowel was retracted towards anterior abdominal wall using fourth arm and multiple nylon stay sutures. These stay sutures were passed through anterior abdominal wall using straight needle and after passing through peritoneal edge, the sutures were taken back out and anchored using artery forceps. The paracaval, retrocaval, precaval, interaortocaval, preaortic, and paraaortic lymph nodes were then dissected. Traction on stay sutures was sequentially increased from outside the abdominal wall as the dissection progressed cranially. This helped in not only increasing the space for retroperitoneal dissection but also formed a mesh preventing the small bowel from obstructing the surgical field. The right renal vein, left renal vein, and bilateral renal arteries were identified defining the upper limit of dissection. The right gonadal vein was dissected until its origin on IVC and was clipped and divided. The lateral limit was defined by bilateral ureters. Complete bilateral RPLND and right pelvic lymph node dissection was achieved robotically. No drain was placed.
The abdomen was desufflated, and the specimen was retrieved from the assistant port. The ports were removed under vision, and the port sites closed.
The total intraoperative time was 4 hours with a blood loss of 100ml. The patient was discharged from the hospital on Day 2 after surgery and the post-operative course was uneventful.
The histopathology revealed 35 lymph nodes, all free of tumour.
Conclusion
Our case highlights the technical nuances, intraoperative meticulous steps and robotic expertise that needs to be followed in a major surgery of this kind to prevent devastating complications. This case also highlights the challenges of robot-assisted RPLND in a patient with NSGCT who had received chemotherapy previously.
RA-RPLND offers several advantages over traditional open RPLND. The use of robotics allows for a faster recovery and more precise dissection of the retroperitoneal lymph nodes, potentially reducing the risk of damage to surrounding vital structures.
Dr. Puneet Ahluwalia
Director and Head - Uro-Oncology and Robotic SurgeryKidney and Urology Institute
Medanta - Gurugram
Uncommon Side Effects of Commonly Used Metronidazole
Metronidazole is a commonly used over-the-counter nitroimidazole antibiotic in India that is widely used for the treatment of infections caused by anaerobic bacteria and protozoa. While metronidazole is generally well-tolerated, it has been associated with rare neurological side effects, including cerebellar toxicity. Cerebellar toxicity refers to the impairment of cerebellar function, leading to symptoms such as ataxia, dysarthria, and nystagmus.
We present a case of metronidazole-induced cerebellar toxicity in a middle-aged patient who presented with symptoms of ataxia and dysarthria. Neurological examination and diagnostic tests, including neuroimaging, confirmed the presence of cerebellar dysfunction. The symptoms resolved gradually after discontinuation of metronidazole, indicating a causal relationship. This case highlights the importance of recognising metronidazole-induced cerebellar toxicity as a potential side effect and the need for close monitoring during treatment.
Case Study
A 54-year-old male patient with no significant medical history presented to the Neurology Department of Medanta - Lucknow with complaints of unsteady gait and slurred speech that had developed over the past 4 weeks. He had a history of intermittent episodes of diarrhoea for the last 2 years for which he used to take metronidazole 500mg thrice daily for 5-7 days every fortnight. He had no history of head trauma, recent illnesses, or use of other medicines.
On examination, the patient had a broad-based, unsteady gait with a tendency to fall to either side. He exhibited dysarthria, characterised by slurred speech and difficulty pronouncing words. There were no signs of cranial nerve abnormalities, sensory deficits or bladder/bowel incontinence; rest of the physical examination was unremarkable.Laboratory investigations, including complete blood count, liver function test, renal function test, and level of electrolyte, showed values to be within normal limits. Magnetic resonance imaging (MRI) of the brain revealed T2/FLAIR hyperintensity in bilateral dentate nucleus while an electroencephalogram (EEG) showed no epileptiform activity.
Considering the temporal relationship between the initiation of metronidazole therapy and the onset of symptoms, a diagnosis of metronidazole-induced cerebellar toxicity was suspected. The antibiotic was discontinued, and the patient was monitored closely. He was then referred to a Gastroenterologist, who diagnosed him with Irritable Bowel Syndrome and started appropriate treatment. Over the course of the next few weeks, the patient's symptoms gradually abated. At his 1-month follow-up visit, he could walk and talk normally again with no residual deficits.
Discussion
The exact mechanism of this toxicity is not fully understood. It is believed to involve the formation of toxic metabolites that impair the function of cerebellar neurons. A systematic review done by Kuriyama, et al. on metronidazole-induced central nervous system toxicity showed that 77% patients had cerebellar dysfunction, 33% had altered mental status and 15% had seizures. Average age of patients was 53.3 years and 64% were male and median duration of metronidazole intake was 54 days. Most patients presenting with cerebellar dysfunction had symptoms like dysarthria, ataxia, dysmetria and nystagmus in decreasing order. About 65% had complete resolution of their symptoms with discontinuation of metronidazole therapy, as seen in our case.
According to Kim, et al, in cases of metronidazole-induced encephalopathy, MRI demonstrates bilaterally symmetrical brain lesions at cerebellar dentate nuclei, dorsal medulla, dorsal pons, midbrain and splenium of corpus callosum. In our case, symmetrical hyperintense focus was noted in dentate nucleus of bilateral cerebellum. A review of dentate nucleus abnormality was done by Bond, et al, which describes various differentials associated with it and the approach towards it.
Conclusion
Metronidazole-induced cerebellar toxicity is a rare adverse effect but should be considered in patients presenting with acute onset cerebellar symptoms during or after treatment for stomach-related issues, especially diarrhoea. Prompt identification and discontinuation of metronidazole can lead to a favourable outcome. Healthcare professionals should be aware of this potential adverse reaction and exercise caution while prescribing metronidazole, particularly in patients with a predisposition to cerebellar dysfunction. Further research is needed to better understand the underlying mechanisms and risk factors associated with metronidazole-induced cerebellar toxicity.
Dr. Vibhor Upadhyay
Associate Consultant - NeurologyInstitute of Neurosciences
Medanta - Lucknow
Dr. Anup Kumar Thacker
Director - NeurologyInstitute of Neurosciences
Medanta - Lucknow
In Focus
MitraClip Valve Repair Technology Used to Treat Two Different Heart Valves Simultaneously
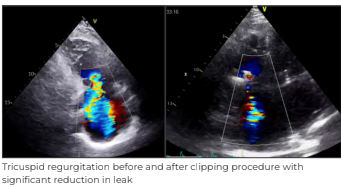
An 87-year-old male with diabetes, hypertension, and hypothyroidism presented to Medanta - Gurugram with the chief complaint of severe breathing difficulty while walking and bilateral swelling in the lower limbs, which are signs of congestive heart failure. He had a history of coronary bypass surgery, done in 1987, followed by a second bypass surgery, done in 2001. He had remained asymptomatic till a few months back. Transesophageal echocardiographic (TEE) evaluation showed non-coaptation of septal and posterior leaflet, massive tricuspid regurgitation, moderately severe mitral regurgitation with preserved systolic function of both left and right ventricle, and moderate pulmonary hypertension.
Tricuspid regurgitation is a condition that occurs when the heart’s tricuspid valve fails to close properly leading to blood flowing back into the right atrium. This along with mitral regurgitation can cause congestive cardiac failure with symptoms of both left- and right-sided heart failure. The condition can be life-threatening if not treated in time.
The patient was optimised on medical therapy for 3 months, but there was not much improvement in his symptoms. In view of his age and previous heart surgeries, he was considered at high-risk for another heart surgery. Hence, considering the risk-benefit ratio, a multidisciplinary team of doctors at Medanta - Gurugram chose the non-invasive treatment methodology of MitraClip valve repair technology to treat the mitral and tricuspid valve leakages.
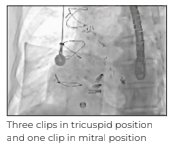
MitraClip treatment is a standard procedure for patients at high-risk from open surgery of mitral regurgitation. In this case, the MitraClip technology was used for treating two different valves of the heart - the mitral and the tricuspid valves - simultaneously for the first time in India and Southeast Asia. Using MitraClip for tricuspid position is technically a demanding procedure as the clip is only designed for the mitral valve; the dedicated tricuspid valve clip is not available in India.
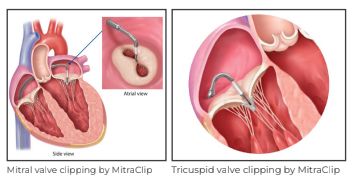
The procedure was performed under general anaesthesia, navigated with the help of advanced 3D echocardiographic (3D Echo) imaging. The procedure was completed in 2 hours with the placement of 1 clip in the mitral position to treat the moderately severe mitral regurgitation, while 3 clips were required to clasp the massive tricuspid regurgitation. The patient was extubated on the same day and stabilised for the next few days. The patient was discharged on postoperative Day 3 with 2 valves repaired without open surgery.
He was able to walk without any symptoms. He has since recovered well and reported significant improvement in his quality of life.
Tricuspid clipping treatment using MitraClip is a new, minimally invasive procedure that has shown promising results in treating tricuspid regurgitation. During the procedure, a small clip is placed on the leaflets of the tricuspid valve to help close it properly.
Using MitraClip to fix both the leaking valves is a unique example of advancement in non-surgical valve therapies at Medanta - Gurugram. Unlike traditional surgeries, mitral valve and tricuspid valve clipping treatment does not require the chest to be opened up, and recovery time is much shorter. Studies have shown that mitral valve repair using MitraClip system is a safe and effective procedure, with many patients experiencing significant improvement in their symptoms of mitral regurgitation.
Dr. Praveen Chandra
Chairman - Interventional and Structural Heart Cardiology Heart Institute
Medanta - Gurugram
Dr. Nagendra Singh Chauhan
Senior Director - Interventional CardiologyHeart Institute
Medanta - Gurugram
Three clips in tricuspid position and one clip in mitral position
Dr. Manish Bansal
Senior Director - Clinical and Preventive CardiologyHeart Institute
Medanta - Gurugram
Welcome Onboard
 Dr. Ankur Nandan Varshney
Dr. Ankur Nandan Varshney
Consultant - Medical and Haemato Oncology
Medanta - Gurugram
Medical and haemato oncologist with expertise in all types of solid tumour chemotherapies, immunotherapies and hormonal therapies. He specialises in advanced bone marrow transplantation and palliative care.
 Dr. Vinit Kumar
Dr. Vinit Kumar
Associate Consultant - Interventional Cardiology
Medanta - Ranchi
Interventional cardiologist with expertise in primary angioplasty, complex coronary interventions, structure heart disease interventions, including ASD, VSD, PDA closure and stenting in addition to heart failure device therapies, including CRTD, CRTP, AICD and dual chamber pacemaker.
 Dr. Ghulam Nabi Maknoo
Dr. Ghulam Nabi Maknoo
Consultant - Interventional Cardiology
Medanta - Gurugram
Interventional cardiologist with expertise in coronary and peripheral angiographies, including primary and complex angioplasties, implantation of temporary and permanent pacemaker in addition to balloon mitral valvuloplasties, 2D and transesophageal echocardiograms.
 Dr. Shubham Shukla
Dr. Shubham Shukla
Associate Consultant - Nephrology and Kidney Transplant Medicine
Medanta - Lucknow
Medical and haemato oncologist with expertise in paediatric haematology and oncology. He specialises in the treatment of all kinds of haematological cancers, including leukaemias, lymphomas, histocytosis and solid tumours including Ewing’s sarcoma, osteosarcoma, rhabdomyosarcoma, hepatoblastoma, Wilm’s tumour, and brain tumours, in addition to benign haematological disorders like thalassaemia, sickle cell disease, immune thrombocytopenia, etc.
 Dr. Amit Kumar
Dr. Amit Kumar
Consultant - Paediatric Haematology and Oncology
Medanta - Patna
Nephrologist with expertise in managing all kinds of kidney diseases, including diabetic kidney disease, hypertension, glomerular disorders and chronic kidney disease. He specialises in haemodialysis and peritoneal dialysis in addition to management of kidney transplant patients.






