THE EXCHANGE | Newsletter - Nov 2023
A Case of Multiple Magnet Ingestion by a Toddler
Ingested neodymium magnets are a serious health hazard for children that carry an extremely high risk of intestinal obstruction and perforation as loops of bowel may get trapped between multiple magnets. We report the case of a child who ingested multiple magnetic beads, and subsequently developed intestinal fistula requiring surgical intervention.
Case Study
A 2.4-year-old child, who ingested multiple magnetic beads, presented to Medanta -Gurugram, and was admitted under the Gastroenterology department of the Institute of Digestive and Hepatobiliary Sciences. The child had ingested three magnetic beads from a toy a month ago. Before coming to Medanta - Gurugram, the parents consulted multiple doctors and were advised to wait and watch after prescribing oral laxatives to be continued till Day 25 post ingestion. On the advice of a local physician, X-ray of the abdomen was performed, which showed that the magnetic beads were stuck in the intestine. They then consulted at Medanta - Gurugram and the child was admitted immediately.
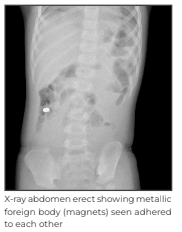
Post admission, X-ray abdomen erect was done to check the position of the magnets. It showed no change and the magnets appeared to be stuck to each other. Under fluoroscopy, three balls were identified while endoscopically one ball was seen adhered to mucosa; this was removed using Roth Net forceps. The other two balls could not be identified in the rest of the colon till up to 25cms of terminal ileum. The possibility of sealed fistula with the other two magnets was considered.
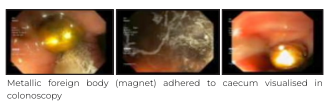
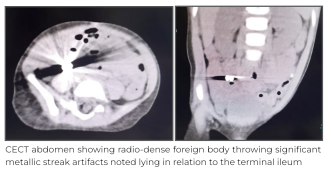
Metallic foreign body (magnet) adhered to caecum visualised in colonoscopy CECT abdomen showing radio-dense foreign body throwing significant metallic streak artifacts noted lying in relation to the terminal ileum X-ray abdomen erect showing metallic foreign body (magnets) seen adhered to each other.
This was followed by a contrast enhanced computed tomography (CECT) scan of the whole abdomen using oral gastrographin. A radio-dense foreign body throwing significant metallic streak artifacts was noted lying in relation to the terminal ileum. Cecum and rest of the large bowel was unopacified and was unremarkable. No significant extra-luminal air to represent perforation was noted in the scan. Due to artifacts, it was not possible to comment if the foreign body was outside or inside the gastrointestinal (GI) lumen.
As these metallic bodies could not be identified even after thorough search on a colonoscopy, the patient was advised diagnostic laparoscopy with foreign body retrieval.
After takin parents' consent, the patient was taken for surgery. The foriegn body was identified and retrieved laparoscopically and the bowel end were repaired. These magnets had created fistula between the caecum and the mid jujunum. Although, classically open surgery is done, we choose the laparoscopic approach to provide benefit of access, magnification and minimal scarring.

His post-operative clinical course was uneventful and he was discharged after establishment
of feeds on Day 7 after the surgery.
Conclusion
Healthcare professionals involved in the care of children should be educated about the serious risks posed by ingestion of magnets from toys. Patients who have ingested magnets may not become overtly symptomatic until a significant degree of bowel injury or even perforation has occurred.
The general consensus within the North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition is that if conservative management is chosen, direct patient observation in a controlled setting should be maintained. In addition, abdominal films and clear ownership of the patient, until such time as passage of the magnets can be confirmed, are vital.
If a child has ingested multiple magnets, and there is no progress in serial X-rays after conservative management then endoscopic retrieval should be done. In case of failed endoscopic retrieval, the magnets should be removed surgically.
Further, we should increase awareness among parents about avoiding toys that have
magnetic beads or small button batteries.
Dr. Neelam Mohan
Senior Director and HOD - Department of Paediatric Gastroenterology, Hepatology and Liver Transplantation
Institute of Digestive and Hepatobiliary Sciences
Medanta - Gurugram
Dr. Shandip Kumar Sinha
Director - Paediatric Surgery and Paediatric Urology
Paediatrics
Medanta - Gurugram
Dr. Sailen Kumar Bana
Associate Consultant - Department of Paediatric Gastroenterology, Hepatology and Liver Transplantation
Institute of Digestive and Hepatobiliary Sciences
Medanta - Gurugram
Medanta@Work
Growth Modulating Surgery in Metabolic Bone Disease
Children with nutritional rickets - the most common metabolic bone disease - usually present in paediatric endocrinology clinics. But, they also seek advice for bony deformities in orthopaedic clinics.
The usual treatment of metabolic bone disease depends on the aetiology. In case of nutritional rickets, calcium and vitamin D supplementation, in the right dose, for a period of three months is sufficient for complete healing. Mild bony deformities tend to correct on their own with the ongoing remodeling in growing children.
Correcting moderate to severe deformities in older children needs orthopaedic intervention.
A decision regarding the timing and type of surgery depends on factors, including the healing stage of rickets, age, remaining growth period, and severity of deformity.
Usually, planned surgeries are done after three to six months of treatment when rickets has healed completely. To decide which type of surgery would be best suited, we need to consider the severity of deformity and the remaining growth period. Surgical corrections become challenging in children nearing the end of their growth spurt.
In such cases, before deciding the right time to do the surgery, we must evaluate whether to wait for healing to be complete - this may result in lapse of important growth period leading to the need for more invasive osteotomies - or intervene early utilising remaining growth period for correction of deformity to save the child from invasive osteotomies. However, the latter poses an increased risk of procedure failure as bones are softer before the healing has completed.
Case Study
A 14-year-old child presented to Medanta - Lucknow with complaints of muscle pain, limping gait, and deformity of the right leg for almost one year.
He had normal growth, pubertal development and did not have a history of any chronic illnesses. His dairy intake was meagre and he hardly had any sun exposure. He did not have any complaints pertaining to the gastrointestinal or renal systems, nor did he take antitubercular (ATT) or antiepileptic drugs.
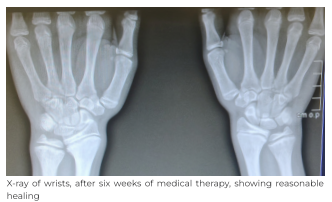
On initial evaluation, he had knobby ends of wrists and tibia with valgus deformity of the right leg. The intermalleolar distance was 13cm and the femorotibial angle on the orthoscanogram was 20°.
Biochemical analysis and initial X-rays were consistent with full-blown rickets. Considering his history, a diagnosis of calcipenic rickets, likely nutritional, was made. He was started on therapeutic does of vitamin D and calcium, and a possible need for surgery was discussed with the family
As the patient was in an advanced stage of puberty with near-closing epiphysis, the need for early growth-modulating surgery and/or the possibility of osteotomy at a later stage was discussed with the family.
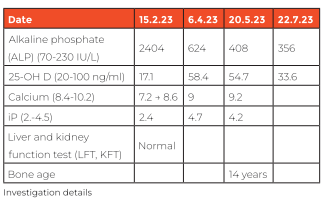
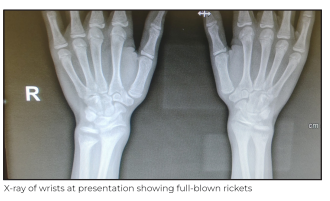
At a six-week follow up, reasonably good healing of rachitic lesions was noted along with
near-normalisation of biochemical parameters. In view of the significant valgus deformity of the right knee along with near-closing epiphysis, it was decided to do a growth modulating surgery to correct the deformity with minimal intervention as literature evidence suggests valgus deformities ≥20⁰ after 9-10 years are unlikely to correct on their own.
In this case’s setting, we took calculated risks on the following points:
1. Doing surgery a bit early, before complete healing of rickets, to buy some important time for growth modulation but at a somewhat increased risk of implant migration.
2. We opted for a comparatively less invasive and simpler intervention, which could have turned out to be totally futile as time for growth modulation was very less or could have provided reasonable results. In the latter scenario, we would have averted more invasive and debilitating osteotomy/osteotomies.
In growth modulating surgery, hemi-epiphysiodesis of one or both sides is done on the convex side of the joint to restrict the growth of epiphyseal cartilage on that side. This, in turn, allows more growth on the opposite side of the cartilage, hence correcting the deformity.
The child underwent right hemi-epiphysiodesis at six weeks of presentation. The surgery
was successful with good clinical outcome and the patient was discharged on Day 1 after the
surgery.

Three-and-a-half months after the surgery, there was visibly significant improvement in the deformity with near-normalisation of intermalleolar distance (7.5cm; normal up to 8cm).
The child was continued on maintenance doses of vitamin D and calcium.
Conclusion
Growth-modulating surgeries in bony deformities have an important role to play, and small
interventions for rickets at the right time may save children from undergoing more invasive
osteotomies at a later stage.
Dr. Lokesh Sharma
Consultant - Paediatric Endocrinology
Paediatrics
Medanta - Lucknow
Dr. Saif N Shah
Director - Orthopaedics
Institute of Musculoskeletal Disorders and Orthopaedics
Medanta - Lucknow
Selective Angioembolisation Helps Check Bleeding after Optical Internal Urethrotomy
Bleeding after an optical internal urethrotomy (OIU) is one of the common complications
after a cold knife incision. While minor bleeding subsides spontaneously and any persistent
bleeding responds well to perineal compression, massive bleeding after OIU is quite rare.
There are very few reported cases of massive bleeding after urethrotomy. In case of massive
bleeding, or refractory bleeding, ultrasound-guided compression and angioembolisation have been described. We report a case of life-threatening bleeding after an OIU that was successfully managed with angioembolisation.
Case Study
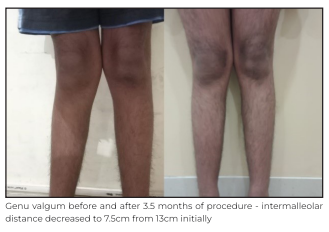
A 59-year-old male was referred to Medanta - Patna with massive per urethral bleeding on Day 5 after an OIU. On evaluation, his vitals were within normal limits with haemoglobin level of 6.4g/dl; other laboratory parameters, such as liver function test and coagulation profile, were also normal. Because of the massive persistent bleeding, a firm perineal and penile compression was applied. One unit of leukocyte depleted packed red blood cells (LDPRBC) was transfused and the patient was kept on observation. However, even after compression, he continued to have episodes of profuse bleeding and clot retention at night. The next day, his haemoglobin was 6g/dl.
One more LDPRBC was transfused followed by a colour Doppler ultrasonography, which showed a pseudoaneurysm around the bulbar urethra.
The patient and his family were told about ultrasound-guided (USG) compression and further conservative management, but they decided to go ahead with computed tomography (CT) pelvic angiography. Angiography showed contrast extravasation from the left bulbourethral artery likely pseudoaneurysm.
Different invasive approaches for management, such as endoscopic fulguration, angioembolisation, and open surgical repair, were explained and discussed with the patient and his family. They opted for angioembolisation because of its minimally invasive nature. Superselective embolisation of the bulbourethral artery was performed via transfemoral approach bilaterally with polyvinyl alcohol particles (300-500 microns).

The procedure went well with good clinical outcome. The bleeding stopped completely after the procedure. Per urethral catheter was removed on Day 2 after the procedure and the patient voided well. On a one-month follow up, there was no episode of bleeding and the patient was voiding well.
Discussion
Urethral stricture can be defined as fixed anatomical narrowing of the anterior urethra resulting in poor flow of urine or difficult instrumentation without mucosal disruption. Internal urethrotomy with cold-cutting knife is one of the frequently-used endosurgical treatments of short-segment non-dense bulbar urethral stricture. Despite the higher recurrence rate as compared to urethroplasty, it is preferred by, both, surgeons and patients because of its minimally invasive nature. The goal of the surgery is to get a larger luminal diameter after healing. Most surgeons prefer to incise the urethra at a 12-o-clock position. Almost always, some degree of bleeding happens after the incision, which resolves spontaneously or through external compression.
Bleeding is the second most common complication of OIU next to recurrence. Massive bleeding, which requires blood transfusion or some invasive intervention, is rare.
In the index case, the patient had a history of recurrent stricture and previous OIU. He presented with bleeding and a significant drop in haemoglobin from baseline (10.4 to 6.4gm/dl), which was managed successfully with selective embolisation. For angioembolisation, the polyvinyl alcohol (PVA) particle was preferred over the coil because there was no specific feeder supplying the pseudoaneurysm. Rather, this pseudoaneurysm was getting fed from multiple tiny branches from bilateral internal pudendal arteries. Before
PVA particles embolisation, the pre embolisation angio from the microcatheter was carefully accessed to make sure there was no other branch getting opacified. Once we ensured that only tiny feeders supplying the pseudoaneurysm are getting opacified only then were PVA particles used to embolise them thus preventing non-target embolisation.
Causes of profuse bleeding after urethrotomy were cited as a deep cut through scar tissue
into the corpus spongiosum, injury to the bulbourethral artery, and a deep cut into corpora
cavernosa. Bulbourethral artery can be injured due to abnormal location because of
previous surgery or anatomical variations.
Location of urethral arteries in the bulbar urethra is found to be at the 1- to 2-o-clock position in 14% of patients; 3- to 4-o-clock in 22%; 5- to 6-o-clock in 17%; 7- to 8-o-clock in 18%; 9- to 10-o-clock in 18%; 11- to 12-o-clock in 11% patients in a study by Chiou et al. Although bulbourethral arteries are symmetrically located at 3-o-clock and 9-o-clock position, asymmetric location in stricture cases were noted by Kishore et al. Abnormal location increases the risk of injury while doing cold knife cutting. Sometimes, a vigorous cut is required to gain the optimal diameter, which can lead to bleeding. These vigorous cuts through dense stricture/spongiofibrosis are found to be unnecessary and it doesn’t help in the prevention of the recurrence of stricture.
There is limited report on massive bleeding post-OIU. Successful management by USG-guided compression has been reported by Attri et al. Compression temporarily stops the bleeding and helps in developing a haemostasis plug, which further converts small pseudoaneurysms in a simple haematoma. USG-guided localisation and compression of small pseudoaneurysm is well described in literature with a moderate success rate. It is also described for high-flow priapism as an alternative to angioembolisation. Only a few cases of
angioembolisation for massive per urethral bleeding after OIU have been reported in literature. After embolisation, bleeding was controlled in almost all cases. But, the transfemoral embolisation is not only invasive, it also requires a lot of expertise, a digital subtraction angiography (DSA) suite, and the burden of additional cost.
Like other invasive procedures, it has its own complications also such as bleeding, pain, haematoma, thrombosis, migration of coil, arterial dissection, impotence, and ischemic stricture. In the index case, no complications were noted.
This case highlights the use of super-selective embolisation in urethral bleeding, which is frequently used to stop bleeding after post-percutaneous nephrolithotomy.
Dr. Avinash Kumar
Senior Consultant
Interventional Radiology
Medanta - Patna
Dr. Prabhat Ranjan
Director - Urology and Kidney Transplant Surgery
Kidney and Urology Institute
Medanta - Patna
Dr. Satish Kumar Ranjan
Associate Consultant - Urology and Kidney Transplant Surgery
Kidney and Urology Institute
Medanta - Patna
Kudos
Congratulations to Mr. Vinodh K (Director - Nursing, Medanta, Gurugram) on being
conferred the Nursing Excellence Award by the Trained Nurses Association of India in New
Delhi, and the Director of the Year 2023 award by Icons of Asia.
These recognitions underline our unwavering commitment and pioneering vision in nursing
leadership.
Welcome Onboard
 Dr. Namrata Sinha
Dr. Namrata Sinha
Associate Director - Onco Pathology
Medanta - Patna
Pathologist with expertise in histopathology, oncopathology, neuropathology, and lymphoreticular pathology. She specialises in immunochemistry, frozen section and cytology.
 Dr. Arun Singh Bhadauria
Dr. Arun Singh Bhadauria
Consultant - Gastroenterology
Medanta - Indore
Gastroenterologist with expertise in managing critical patients with liver failure,
pancreatitis, inflammatory bowel disease, and intestinal bleeding. He specialises in
diagnostic and therapeutic endoscopy, colonoscopy, endoscopic retrograde
cholangiopancreatography (ERCP), endoscopic ultrasound (EUS), and endoscopic surgeries.
 Dr. Kunwar Ashish Singh
Dr. Kunwar Ashish Singh
Associate Consultant - Hepatology
Medanta - Gurugram
Hepatologist with expertise in managing liver failure syndrome, non-alcoholic fatty liver
disease and viral hepatitis. He specialises in liver transplantation, critical care hepatology,
diagnostic and therapeutic endoscopy with special interest in endo hepatology.
 Dr. Bharti Arya
Dr. Bharti Arya
Associate Consultant - Ophthalmology
Medanta - Gurugram
Ophthalmologist with expertise in vitreo-retina medical and surgical services, retinopathy of
prematurity (ROP) services and cataract surgery.
 Dr. Richa Tiwari
Dr. Richa Tiwari
Associate Consultant - Paediatrics
Medanta - Lucknow
Paediatrician with expertise in treating epilepsy, neuroinfections, neuroimmunology,
neuromuscular diseases and neuro developmental diseases including autism, attention-
deficit/hyperactivity disorder (ADHD), cerebral palsy.
 Dr. Rohini R Nair
Dr. Rohini R Nair
Associate Consultant - ENT, Head and Neck Surgery
Medanta - Patna
ENT surgeon with expertise in performing varied otological, endoscopic nasal and laryngeal
in addition to head and neck surgeries. She specialises in managing allergies and vertigo.
 Dr. Rajani Kant Kumar
Dr. Rajani Kant Kumar
Associate Consultant - Cardiac Surgery
Medanta - Patna
Cardiac surgeon with expertise in performing surgeries for adult structural heart defects and
congenital heart defects.






