THE EXCHANGE | Newsletter July 2019

Adenoid Cystic Carcinoma of Paranasal Sinuses A Therapeutic Challenge
Adenoid cystic carcinoma (ACC) accounts for nearly 3 to 5% of all head and neck malignancies. It is characterized by an intermediate growth rate, probability of perineural infiltration (PNI) and frequent lung / bone metastasis. The overall survival (OS) rates of localized ACC that originate in the major salivary glands and minor oral cavity salivary gland are 93.9% and 92.4% respectively, whereas survival rates for metastatic disease are 43.3% and 55.4% respectively. However, ACC of the paranasal sinuses (PNS) and skull base represents pathology with distinct clinical implications. These tumours are typically diagnosed late, and their proximity to vital structures (e.g. dura, brain, orbit, and cranial nerves) makes adequate oncological resection difficult. Another characteristic of ACC of the paranasal sinuses is the perineural infiltration (PNI), with an incidence of over 50%. Due to the high propensity of local invasion to adjacent vital anatomical structures (i.e. cranial nerves) and late diagnosis, ACC is associated with poor prognosis, intracranial extension, and positive surgical margins. Surgery represents the mainstay of treatment in nearly all patients of ACC. Publications by Stewart et al in 1968 and King & Fletcher in 1971 suggest that surgery followed by adjuvant radiation therapy (RT) provides superior disease control compared to either modality alone. However, the role of postoperative RT needs to be defined in large randomized trials. Although some physicians advocate RT for essentially all patients with adenoid cystic carcinoma of the head and neck, others reserve RT for only those with unfavourable features such as advanced disease, PNI or positive surgical margins. For inoperable tumours, RT alone is the standard of care.
Case study
A 45-year-old male was evaluated at another hospital for complaints of left temporal throbbing headache since 6-7 months. He was diagnosed hypertensive at the same time. The patient was started on antihypertensive and migraine medications by a local physician but he had no relief in his symptoms. He presented to Neurology OPD at Medanta in January 2014, a week after he developed numbness over the left side of face. A CT scan of face and neck, and a subsequent contrast enhanced MRI Brain were done which showed a soft tissue mass lesion involving floor and left lateral wall of sphenoid sinus. Anteriorly, the mass was extending into the left posterior nasal cavity Fig 1(A). There was contiguous infiltration of left masticator space Fig 1(B). Disease was spreading along the left mandibular nerve with widened foramen ovale Fig 1(C), reaching up to anterior part of Meckel's cave possibly involving the gasserian/trigeminal ganglion and cavernous sinus Fig 1(D). Superiorly above the masticator space, there was infiltration of the dura along the floor of middle cranial fossa. However, no infiltration/edema of the underlying temporal lobe was seen Fig 1(E). Involvement of pterygopalatine fossa, foramen rotundum reaching upto the right infraorbital fissure and orbital apex was also noted Fig 1(F).
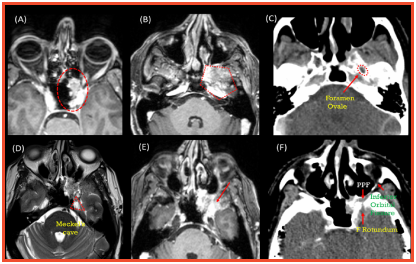
Figure 1: Initial disease extent as seen at the time of presentation on CECT and CE MRI Brain
Patient was referred to Head & Neck Oncology Department for further management where a nasoendoscopy was performed under general anesthesia in which a proliferative lesion in left lateral wall of sphenoid sinus was visualized. Biopsy taken from the lesion was suggestive of adenoid cystic carcinoma. After a multi-disciplinary Tumour Board discussion, patient was planned for definitive radiation therapy as the disease was quite extensive and surgery would entail the risk of loss of vision with increased likelihood of R2 resection, thus still requiring radiation therapy in the adjuvant setting. It is seen that a dose of 60-66Gy/30-33# over six weeks results in long periods of remission. The target volume must include the gross disease with potential sites of microscopic disease extension. In the present case scenario since there was evidence of gross perineural spread along the mandibular nerve or 3rd division of Vth/trigeminal nerve up to the Meckle's cave and cavernous sinus, our target volume included the entire course of the trigeminal nerve. In orderto cover the entire course of the mandibular division of trigeminal nerve upto the Meckel's cave to account for the gross and microscopic disease extension, our target volume extended cranially upto the cavernous sinus and critical structures like left optic nerve and optic chiasm were within the treatment volumes.
Since tolerances of optic structures is 54Gy max dose and <60 Gy to 1% volume, it was difficult to achieve these dose constraints without compromising the doses to the target volume. Thus, RT was planned in two phases. In phase 1: 50Gy/25 #/5weeks @2GY/# were delivered on LINAC under daily image guidance. Thereafter, reassessment scan was performed and boost dose 18Gy/3# @6Gy/Fraction was delivered with Cyberknife to the gross residual disease, such that max dose to left optic nerve and optic chiasm were 8.1Gy and 5.5 Gy respectively. With Cyberknife it was possible to achieve 50 % dose reduction within 2.63mm from the target so that the closely located optic apparatus gets doses within the tolerance limits. Treatment was completed in March 2014. Follow up MRI Brain with contrast done after three months of completion showed complete radiological response. The latest contrast enhanced MRI brain, done after five years of treatment completion, shows that the patient is still in remission. However, there is ‘Swiss Cheese’ enhancement noted around the previously treated tumour bed, suggestive of radiation necrosis as shown in Fig 2.
Patient has been doing well for the last five years. His present visual acuity, swallowing capability, speech and aesthetics are all preserved. He is able to carry out all his pre - morbid activities like travelling independently. Although, he develops frequent nasal infections for which he is being managed conservatively with oral antibiotics. He is also asymptomatic for the radiation necrosis currently. From the available literature of radiation necrosis after brain radiosurgery, it has been observed that most necrotic sites remain asymptomatic and heal with gliosis over time i.e. weeks to months. If patient becomes symptomatic, depending upon the severity, oral or injectable steroids, hyperbaric oxygen therapy (HBOT), or in extreme cases, craniotomy and removal of the necrotic component can be considered. For the patient’s secondary pan hypopituitarism, he is being treated by the Endocrinology team. He is on hormone replacement therapy with Tab Eltroxin 62.5 mg, Tab Hisone 7.5-5-2.5 gm and Inj Testosterone.
In conclusion, radiotherapy alone is effective for treatment of ACC of PNS for patients who are not candidates for surgery due to disease location or extent at time of presentation. Cyberknife is an efficient radiation system with robotic maneuverability that allows clinicians to deliver precise treatment with pin point accuracy and minimal collateral damage.
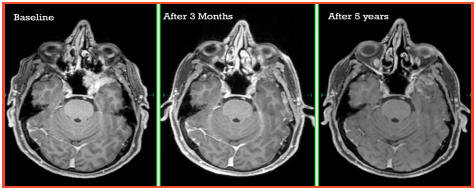
Figure 2: Serial response assessment CE MRI Brain scans
https://www.medanta.org/dr-tejinder-kataria/
Bariatric or Metabolic Surgery Weight Loss is Merely a Side Effect
Bariatric surgery is a term typically associated with 'weight loss surgery'. Factually, however, for a lot of patients bariatric surgery is not about weight loss but treatment of several weight associated diseases. And losing weight is just a healthy side effect. Common belief among doctors and patients is that body fats are removed during the surgery, similar to a cosmetic or body contouring surgery such as liposuction. It is for this reason that Dr Rubino and group in a position statement for the International Diabetes Federation (IDF) put forth the term 'Metabolic surgery', defined as - a set of gastrointestinal operations used with the intent to treat diabetes (diabetes surgery) and metabolic dysfunctions (which include obesity). Misconceptions about risks and benefits of the surgical treatment have acted as a barrier for both patients and physicians to seek or recommend this surgery.
Who is metabolic surgery for?
Metabolic surgery typically helps patients who are more than about 25 Kg over their ideal body weight. The surgery positively impacts those who have other metabolic problems including diabetes.
Here we review two of our patients who underwent this surgery for reasons other than just obesity.
Case study
A 55-year-old female was referred to Medanta from Lucknow with extensive obesity related problems including obesity hypoventilation syndrome and severe obstructive sleep apnea with pulmonary arterial hypertension. She was incapable of even walking up to the bathroom. She needed continuous oxygen support. She had an extremely poor quality of life. At her height of 4' 11”, she weighed 86 Kg with Body Mass Index of 40 kg/m2. Even though her excess weight was only 25-30 Kg, she was suffering from extensive obesity related problems. Ultrasound revealed Grade 3 fatty liver and Fibroscan was suggestive of early chronic liver disease due to NASH. After admission, she was evaluated with opinion from several specialists including pulmonologist, cardiologist, hepatologist, anesthetist, and her baseline condition was optimized as far as possible in preparation for metabolic surgery. She was started on continuous BiPAP, medically managed with diuretics and diet intervention. Since there was not much hope of her escaping the vicious cycle of medical problems, she was counselled for metabolic surgery. The laparoscopic sleeve gastrectomy was uneventful and she could be extubated and transitioned to BiPAP immediately post-surgery. She was monitored in ICU for a day and then shifted to ward. She had a smooth postoperative recovery and was gradually weaned off oxygen support. At two-month follow up, she walked into the OPD without needing a wheel chair. A positive side effect of the metabolic surgery was that apart from an extensive improvement in her medical conditions and quality of life, she additionally lost 12 Kg weight.
Case study
A 65-year-old male from Dehradun came to Medanta suffering from the triad of obesity, abdominal hernia and symptomatic gallstone disease. At 117 Kg and a Body Mass Index of 41 kg/m2, he carried an increased risk of complications. He had been unsuccessful in losing weight and was also suffering from pain in back and joints. Obesity also put him at an increased risk of hernia recurrence in future. After thorough preoperative evaluation, he underwent bariatric surgery along with cholecystectomy and umbilical hernia repair. He was extremely motivated and started walking the evening of surgery itself and after an uneventful recovery, he could be discharged within two days. At three-month follow up, his back pain and joint pain had improved. He had started regular cycling and brisk walk. His hernia stayed fixed and as a healthy side effect, he shed 37 Kg weight.
Myth busters
Myth: Bariatric surgery induces weight loss because patients can't eat after surgery.
Fact: Patients go back to eating normal food such as roti, dal, and vegetables soon after surgery. However, hormonal changes such as reduction in the appetite hormone 'Ghrelin' gives them a feeling of fullness after consuming small meals. The food intake and calorie consumption is thus reduced. Changes in insulin like hormones mean that calories are burnt more efficiently.
Myth: Patients re-gain weight after surgery.
Fact: Most patients are able to keep the weight off and only a small fraction regain some weight over several years if they don't follow a healthy diet and exercise routine.
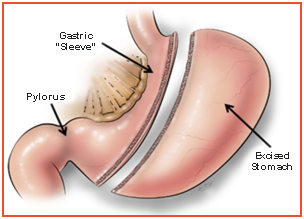
Myth: Fat is removed from the body.
Fact: Bariatric surgery is not a cosmetic surgery like liposuction but a metabolic surgery wherein the stomach and GI tract are operated upon. On average, patients lose about 60% to 70% of their excess weight in a few months following surgery before their weight stabilizes.
Myth: Patients become weak post-surgery.
Fact: Most patients are able to start walking regularly and don't feel weak. Post-op, they are recommended a high protein diet, multi-vitamin, calcium and plenty of fluids. Vitamin levels are monitored at three-month follow up, and then annually as a part of health check on follow up visit.
Myth: Bariatric surgery has a lot of complications
Fact: Bariatric surgery carries the same risks as any other routine surgery like gallbladder surgery. It is done only after an extensive risk assessment. The minimally invasive technique also results in quick return to normal activity. In fact, patients feel very active within two weeks of surgery and exercise conveniently thereafter.