Robotic-assisted cystectomy
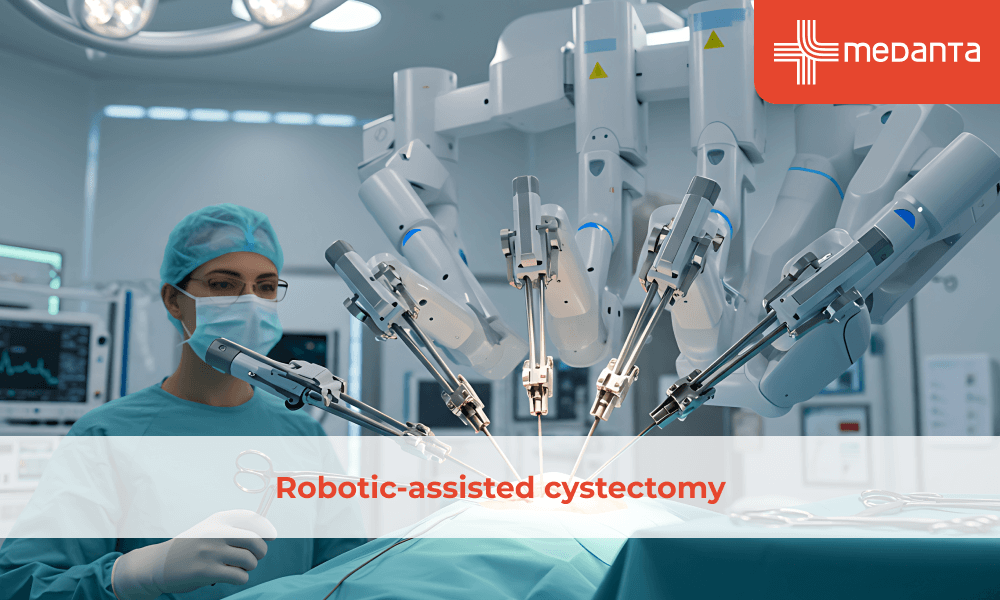
TABLE OF CONTENTS
Robotic-assisted cystectomy has witnessed a remarkable 30-fold increase in adoption since its introduction in 2003, rising from less than 1% to 18.5% of all cystectomy procedures by 2012. This surgical technique has emerged as a preferred choice for treating muscle-invasive bladder cancer and high-risk non-muscle-invasive bladder cancer, mainly due to its minimally invasive nature.
Compared to traditional open surgery, this advanced procedure offers significant advantages, including 40% more lymph nodes recovered, reduced blood loss, and fewer major complications. With an average hospital stay of 6 days versus 8 days for open surgery, patients typically experience better outcomes and improved quality of life, mainly when performed at high-volume medical centres.
Let's explore the essential aspects of robotic-assisted cystectomy, including the procedure details, the recovery process, potential risks, & factors to consider when deciding if this surgical option is suitable for specific cases.
Robotic-assisted cystectomy stands as a minimally invasive surgical technique that matches the cancer removal success rates of traditional open surgery. Through this advanced procedure, surgeons remove the bladder and redirect the urinary tract using a sophisticated surgical robot system.
The surgical process involves a robotic console where the surgeon maintains complete control of the instruments. A high-magnification camera coupled with a computer system provides surgeons with detailed, three-dimensional, high-definition views inside the patient's body. Furthermore, the robotic arms offer enhanced manoeuvrability beyond human capabilities, operating through small incisions with remarkable steadiness and precision.
Initially introduced in 2003, this surgical approach has steadily gained acceptance worldwide as a reliable treatment option. The procedure demonstrates several notable advantages over conventional methods:
Reduced blood loss during surgery
Shorter hospital stays
Better rates of positive margins
Enhanced lymph node recovery rates
Accelerated bowel recovery
Decreased need for pain medication
The surgical robot is an extension of the surgeon's expertise rather than an autonomous system. At the console, the surgeon directs the robotic instruments with precise movements while the robot's steady hands eliminate even minimal unwanted movements. Additionally, the system allows for smaller incisions in the abdomen, filled with carbon dioxide, to create adequate working space for the surgical team.
Studies indicate that robotic-assisted cystectomy with intracorporeal urinary diversion shows particular benefits for elderly patients. The completely minimally invasive nature of the procedure results in smaller incisions, reduced post-operative pain, and faster bowel recovery. Moreover, high-volume medical centres performing this procedure report significantly reduced risks of major post-operative complications.
Recent comparative research spanning 10 years demonstrates that robotic-assisted cystectomy achieves comparable oncological outcomes to open surgery in terms of recurrence-free, progression-free, and overall survival rates. The procedure maintains quality of life scores similar to traditional approaches, though patients receiving robotic intracorporeal urinary diversion report improved outcomes.
Despite its advantages, the procedure presents certain challenges. Surgeons face a learning curve owing to its complex nature. The operation typically requires longer operative times and involves higher costs than traditional methods. However, these factors have not hindered its growing adoption, as the benefits often outweigh the challenges for suitable candidates.
Preparing for robotic-assisted cystectomy involves several crucial steps that ensure optimal surgical outcomes. The medical team conducts thorough evaluations before proceeding with this advanced surgical approach.
Before the Procedure
Patients undergo comprehensive medical assessments, specifically focusing on cardiac and respiratory functions. Blood tests, imaging studies, and detailed discussions about medical history form essential components of preoperative preparation.
The surgical team provides specific instructions regarding the following:
• Medication adjustments
• Dietary restrictions
• Physical activity guidelines
• Personal hygiene protocols
Procedure
The surgical process begins with the patient under general anaesthesia. Small incisions, typically 8-12 millimetres in size, allow for the insertion of robotic instruments. The surgeon positions these instruments through carefully placed ports in the patient's abdomen.
The surgeon maintains complete control at the surgical console while viewing magnified 3D images of the surgical site. The robotic system translates the surgeon's hand movements into precise micro-movements of the surgical instruments inside the patient's body.
The procedure follows these key stages:
Careful separation of the bladder from surrounding structures
Removal of lymph nodes from specific areas
Creation of a new pathway for urine drainage
Meticulous reconstruction of the urinary tract
Recovery and Post-procedure Care
Post-operative recovery focuses on the gradual resumption of normal activities. Most patients start walking within 24 hours after surgery. The medical team monitors vital signs, manages pain, and ensures proper wound healing.
Recovery milestones typically include:
Resumption of liquid diet within 48 hours
Removal of surgical drains after 3-5 days
Hospital discharge between 5-7 days post-surgery
Return to normal activities within 4-6 weeks
The medical team provides detailed instructions for home care, encompassing wound management, dietary guidelines, and activity restrictions. Regular follow-up appointments allow for monitoring recovery progress and addressing any concerns.
Physical therapy often plays a vital role in recovery, helping patients regain strength and mobility. The rehabilitation program adapts to individual progress, ensuring a safe & effective return to daily activities.
Patients receive specific guidance about:
Pain management techniques
Proper incision care
Warning signs that require immediate medical attention
Dietary modifications
Exercise restrictions and recommendations
Maintaining open communication with the healthcare team remains crucial throughout the recovery period for optimal healing and successful outcomes.
Determining suitability for robotic-assisted cystectomy requires careful evaluation of several medical factors. Patients who qualify for open radical cystectomy generally make suitable candidates for this robotic procedure.
Doctors consider specific conditions that might affect the procedure's success. Certain physical characteristics warrant additional consideration:
Body mass index above 30 kg/m2
Presence of extravesical disease
Bulky lymphadenopathy
Previous pelvic radiation or trauma
Prior vascular or distal colorectal surgery
Although these conditions present challenges, experienced surgeons can achieve successful outcomes through careful surgical planning and management.
Some medical conditions absolutely rule out robotic-assisted cystectomy. These include:
Intra-abdominal adhesions preventing port placement
Inability to tolerate pneumoperitoneum
Difficulty maintaining the required 30-degree Trendelenburg position
Uncorrected bleeding disorders
Disease extending into surrounding pelvic structures with bladder fixation
For patients with localised disease, a thorough preoperative medical assessment becomes essential. This evaluation focuses on:
Functional status assessment
Identification of bleeding disorders
Evaluation of pulmonary function
Assessment of cardiac health
For patients deemed unsuitable for robotic surgery, alternative treatment options exist. Trimodal therapy, comprising maximal transurethral bladder tumour resection followed by chemotherapy and external beam radiation, offers an alternative approach.
The decision to proceed with robotic-assisted cystectomy ultimately depends on careful evaluation of these factors, alongside consultation between the surgical team and patient. Success rates remain comparable to traditional open surgery, with added benefits of reduced blood loss, decreased pain medication requirements, and typically shorter recovery periods.
Like any major surgical procedure, robotic-assisted cystectomy carries certain risks that patients should understand. Recent studies from multiple medical institutions reveal significant data about post-operative complications.
The most frequent complications fall into three main categories:
Gastrointestinal complications (27%)
Infectious complications (23%)
Genitourinary complications (17%)
Sexual side effects present another consideration. Men might experience difficulties with erections plus will no longer produce semen following radical cystectomy. Women might encounter discomfort during intercourse, primarily because the procedure sometimes involves partial removal of vaginal tissue.
Several factors influence the likelihood of experiencing complications. Research shows that increasing age, neoadjuvant chemotherapy, plus blood transfusion requirements serve as independent predictors of both minor plus major complications.
Changes in urination patterns commonly occur after surgery. Following partial cystectomy, patients typically need more frequent bathroom visits because of reduced bladder capacity. For radical cystectomy patients, urination ability depends entirely on the type of reconstructive surgery performed.
The mortality rates remain relatively low, with 30-day mortality at 1.3% plus 90-day mortality at 4.2%.
Recent data shows that high-volume medical centres demonstrate better outcomes plus lower complication rates. Furthermore, proper patient selection plus experienced surgical teams significantly reduce the risk of major post-operative complications.
Robotic-assisted cystectomy stands as a significant advancement in bladder cancer treatment, offering patients notable benefits while maintaining comparable success rates to traditional surgery. Medical evidence supports its effectiveness through reduced blood loss, shorter hospital stays, and enhanced lymph node recovery rates.
Patient selection remains crucial for optimal outcomes. Though the procedure presents certain challenges like longer operative times and higher initial costs, experienced surgical teams at high-volume medical centres consistently achieve excellent results. The recovery process typically spans 4-6 weeks, during which patients gradually return to their normal activities.
Success rates match those of conventional surgery, particularly when performed at specialised medical centres with experienced surgical teams. Though complications can occur, proper patient screening and careful surgical planning help minimise these risks. The procedure continues to evolve, backed by growing evidence of its long-term effectiveness in treating bladder cancer.
The future looks promising for robotic-assisted cystectomy as surgical techniques advance and more medical centres gain expertise. Patients considering this procedure should discuss their specific case with qualified medical professionals who can evaluate individual suitability and potential outcomes.
Is robotic surgery safe?
Studies spanning the past decade demonstrate improved surgical outcomes with robotic systems versus open surgery. The surgeon maintains complete control throughout the procedure, directing every movement of the robotic instruments.
What happens during the procedure?
The surgical system serves as a sophisticated tool that assists surgeons. Through tiny incisions, the surgeon operates using a console that provides high-definition, three-dimensional views inside the body. The robotic arms translate the surgeon's hand movements into precise micro-movements.
Will I experience pain during surgery?
Patients receive general anaesthesia throughout the surgery, ensuring they feel no discomfort. Post-operative pain varies among individuals, yet most patients report reduced bleeding plus fewer complications in comparison to traditional surgery.
What advantages does robotic surgery offer?
The minimally invasive nature of the procedure provides several benefits:
Smaller incisions- leading to reduced scarring
Minimal blood loss
Shorter hospital stays
Faster recovery time
Decreased need for pain medication
What potential complications should I know about?
Possible complications include:
• Nerve damage plus compression
• Rare instances of robotic malfunction
• Situations requiring conversion to open surgery, primarily in cases with extensive scar tissue from previous operations
How long does recovery take?
Recovery periods vary based on individual circumstances. Most patients experience:
• Hospital stays averaging 7-8 days
• Return to normal activities within 4-6 weeks
• Gradual improvement in mobility plus function
What factors determine if I'm suitable for this procedure?
Suitability depends on several factors:
• Overall health condition
• Type of surgery needed
• Surgeon's expertise
• Technical considerations
What happens if complications arise during surgery?
In rare cases where complications occur, surgeons might need to convert to traditional open surgery. The surgical team prepares for such possibilities, ensuring patient safety remains the primary focus.





