
THE EXCHANGE | Newsletter January 2023
A Knowledge Sharing Initiative by Medanta
Dr. Randeep Guleria joins Medanta as
Chairman - Institute of Internal Medicine and Respiratory & Sleep
Medicine and Director - Medical Education
Medanta welcomes Dr. Randeep Guleria, a globally renowned pioneer in pulmonary medicine, sleep and
metabolic disorders. Prior to joining Medanta, he was the Director of AIIMS, New Delhi, where he served as a
faculty member for over three decades.
A recipient of the prestigious Padma Shri and Dr. B.C. Roy Awards, Dr. Guleria is known for his exceptional work in the fields of lung cancer, asthma, COPD, respiratory muscle functions and sleep disorders. He is credited with setting up a dedicated Department of Pulmonary Medicine and Sleep Disorders at AIIMS, New Delhi, in 2011.
Dr. Guleria has been a member of the World Health Organization’s (WHO) Scientific Advisory Group of Experts (SAGE) on immunisation and influenza vaccination, and the International Atomic Energy Agency (IAEA) onradiation protection. He is actively involved in management of outbreaks of infectious diseases, such as dengue,H1N1 and, more recently, COVID-19 in India. Dr. Guleria has contributed over 400 papers in reputed international and Indian journals, 49 chapters in various prominent books, and has delivered over 200 lectures in India and abroad.
Tête-à-Tête
Q. Tell us something about your formative years.
I was born in Dharamshala, Himachal Pradesh, in a family of doctors and army officers. While I do have fond memories of growing up in the hills, our family relocated to Delhi, specifically to the AIIMS campus, where my father joined the institute as part of the first batch to pursue DM cardiology in India. This was the early AIIMS had just started, and it was like a close-knit family where all clinicians knew each other and so did their families.
Since it was a hub of academic brilliance, one was at the receiving end of lot of academic pressure. I did my schooling at St Columbus, a missionary school in Delhi, where there was a lot of focus on moral values and ethics alongside academics.
Q. What inspired you to become a doctor?
A doctor and a very passionate academician, my father had a big influence on me and my career choice. His focus on clinical and holistic medicine, in an era when diagnostics as a decision-making tool was not so evolved, was very inspiring. We saw him attend to patients at all hours. He was also a committed teacher; I still come across senior doctors who tell me that they remember his lectures fondly. Also, growing up in the AIIMS campus, with a close network of doctors, was a big influence.
Q. If you weren’t a doctor, what would have been your alternative profession of choice?
I would have certainly joined the Indian Armed Forces. All my maternal uncles were decorated Army officers. I cleared the Army entrance exam twice, but opted out both times. The first time was when I cleared the NDA exam and was booked on a train, bailing out was a last-day, last-minute decision. The second time was when I got selected in the Army Medical Corps, but chose to lead a civilian life.
Q. Is there any particular clinical experience that has had a lasting impact on you?
Each patient is unique and teaches you something. Over the years, I have learnt a lot from my patients by looking at them holistically. This one time, a middle-aged lady, who had been operated for breast cancer, came to me with a follow-up PET scan that showed lesions in the lungs and nodes in the chest. Purely based on this PET scan, she had been told by another doctor that her cancer had spread and that she only had another month to live. Depressed and anxious, she met me for a second opinion. I saw the scan and assured her that it was a case of tuberculosis as breast cancer does not spread in areas indicated in the scan. She took multiple confirmatory opinions and returned two months later. This time, she and her family were positive, upbeat and grateful. This instance has stayed with me and I often share it with my students to emphasize the importance of looking at a patient as a whole, and not just as a bunch of reports and scans. This is how the science of medicine also becomes an art.
Q. Is medicine an art or science for you?
Medicine is both an art and science. As students of medicine, we are trained in newer techniques, modalities of treatment and technologies. As doctors, it is important to constantly learn and upskill. We are making great strides in areas of robotics, artificial intelligence and big data. But technology should only be treated as an enabler.
Clinicians should never forget to look at the patient holistically. Technology can never substitute a doctor’s observation, their empathetic hearing and knowledgable assurance, which are essential to caregiving. This is the art part of medicine. Unfortunately, nowadays, in overloaded superspecialty OPDs, we see this human touch missing.
We need to understand that diseases don’t affect just one organ, and that patients can’t be viewed as an organ that needs treatment. We should look at the patient as a whole, and treat them with an all-encompassing approach. I have seen patients who have been treated for heart problems while lesions in their lung, that were more dangerous, were totally overlooked. I urge all young and budding clinicians to not ignore the critical aspect of holistic caregiving, and respect the trust and faith that patients put in us.
Q. What do you aspire to do next?
I just wrapped up a very demanding administrative assignment in the government sector as the Director of AIIMS, New Delhi, the second half of which was spent in responding to the challenges of the COVID-19 pandemic. I am a clinician at heart, so I would now like to focus on patient care and teaching. I would also like to read a lot more and travel, both of which are my leisure time pursuits. I have not had the luxury to indulge in either for many years.
Q. What’s been your most recent and interesting non-clinical, non-academic pursuit?
After retiring from AIIMS, New Delhi, and with some free time at my disposal, I have finally been able to catch up on some non-academic reading, which I haven’t been able to do in years. I grew up reading Agatha Christie and Perry Mason. More recently, I’m leaning more towards philosophy. I last read Sapiens and The Book of Joy.
Medanta@Work
A First in Uttar Pradesh
Emergency Liver Transplant Saves Life of 3-year-old Girl
Acute liver failure (ALF) is a critical life-threatening condition. It is defined as rapid development of liver dysfunction associated with onset of hepatic encephalopathy (HE) within eight weeks of the appearance of first symptoms in the absence of pre-existing liver disease. Globally, viral hepatitis infections are responsible for majority cases of ALF. Hepatitis A and E are common in developing countries, while Hepatitis B is a common cause of ALF in some Asian and South American countries. In developed countries, drug-induced liver injury, especially with paracetamol, accounts for approximately 50% cases. ALF is further complicated by rapid development of coagulopathy, jaundice, and the potential to rapidly progress to multi-organ failure. Patients with severe hepatic encephalopathy require elective ventilation. In spite of best efforts, progression to cerebral edema and intracranial hypertension may be a feared outcome, unless an urgent liver transplant is performed.
Various prognostic evaluation systems have been used to identify candidates for transplantation. The most commonly used evaluation systems are King’s College criteria with a sensitivity of 68-69% and a specificity of 82-92%. Various other criteria have been defined, including Sequential Organ Failure Assessment (SOFA), Acute Physiology and Chronic Health Evaluation (APACHE), ALF study group index, serum lactate, serum phosphorus, alpha-fetoprotein levels, factor V and VII/V ratio etc. Survival after ALF is multifactorial and depends on etiology, grade of coma on admission and the absence of complications. All these factors can be regarded as pieces of a mosaic than definite criteria. Here, we present a case of acute liver failure, secondary to Hepatitis A in a child.
Case Study
A 3-year-old girl was brought to Medanta-Lucknow from another tertiary care facility after 12 days of admission. Despite medical management, her condition had deteriorated from initial mild fever, jaundice, drowsiness and lethargy to deep coma. She was put on a ventilator and had an episode of generalised tonic-clonic convulsions. Her family was informed that an urgent liver transplant is the only hope of survival.
The baby presented in a very sick condition and had severe jaundice (Total Bilirubin 21.2 mg/dl) with metabolic acidosis (pH 7.2), severe coagulopathy (INR 7.38) and hyperammonaemia (73 umol/L). On examination, her pupils were only sluggishly reacting to light and the child was posturing with Glasgow Coma Scale (GCS) score of E1V1M2. Her symptoms were suggestive of impending brain death due to raised intracranial pressure (ICP). Rapid stabilisation of the baby and ICP lowering manoeuvres – head-end elevation, hyper ventilation, 3N saline, mannitol were initiated by the ICU and the paediatric gastroenterology teams.
The mother of the baby was identified as a compatible liver donor, and after her consent, a battery of blood and radiological tests, including a computed tomography (CT) scan to check liver anatomy, liver volume and various medical clearances, were performed within a matter of a few hours.
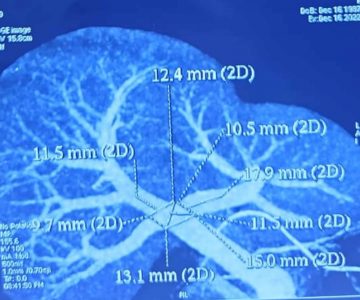
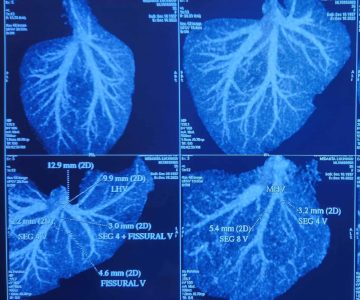
The Emergency Authorisation Committee was called to clear all legal matters pertaining to a liver transplant. Just before the transplant, an electroencephalogram (EEG) and CT brain were performed to rule out brain stem herniation and confirm brain activity to avoid a futile transplant. The Liver Transplant Team from Medanta-Gurugram flew in and the transplant began on November 20 – within a few hours from the time the family consented for a transplant.
Left lateral segment from the mother’s liver was removed and transplanted into the patient’s body. A total of 275 gm of the left lobe was procured with graft-recipient weight ratio (GRWR) 2.1 and preserved in 1,000 ml IGL solution. Hepatic artery, hepatic veins and bile ducts were joined under 3X and 2.5X magnification. Cold ischemia time was 47 minutes and warm ischemia time 31 minutes. One packed red blood cells (PRBC) was used during the procedure; no platelet or cryo was required.
During this challenging operation, the anaesthesia team stabilised the patient and maintained blood pressure haemodynamically. Intra-operative Doppler was performed to confirm blood flow to the new liver. The explanted liver showed features of acute liver necrosis.
The surgery was uneventful and the baby responded well to the procedure with good clinical outcome. With the new liver working, the ammonemia and acidosis improved and the brain swelling reduced; GCS rapidly improved to E4VTM6 and, only 12 hours after the procedure, the baby opened her eyes – first time after a week. The patient was removed from ventilator on Day 2 of surgery and discharged on Day 10 in a stable condition. On follow up, she was doing well.

The outcome is attributable to the well-coordinated efforts of a highly competent team of liver transplant surgeons, hepatologists, anaesthetists, technicians and nurses supported by state-of-the-art infrastructure.
Given the complex presentation and potential for rapid deterioration of patients with ALF, it is essential to have an organised and comprehensive approach, including timely referral to a liver transplant centre. Evaluation for transplantation should involve a hepatologist, transplant surgeon, cardiologist, neurologist, and infectious disease specialist, if warranted, as well as a social worker and transplant coordinators. No time should be wasted for candidates who meet all the transplant criteria. Survival of patients with ALF has significantly improved from 16% to 62% since the introduction of liver transplantation. ALF as an indication for liver transplant was adopted in the 1980s by the National Institutes of Health (NIH). Currently, ALF accounts for approximately 8% of all liver transplants, as per data from the Scientific Registry of Transplant
Recipients (SRTR) and Egyptian Liver Transplant Society (ELTS).
Complex Reconstructive Surgery to Treat Facial Nerve Palsy
Facial nerve palsy is a condition in which there is weakness or complete loss of function of facial muscles leading to facial asymmetry, loss of facial expressions, and difficulty or inability to close eyes completely. This commonly results from unrecovered or partially recovered Bell’s palsy or due to surgical ablation of facial nerve, and leads to significant functional, aesthetic and psychological impairment. The objectives of reconstruction in such cases are to rehabilitate the patient both socially and functionally by restoring facial symmetry – static and dynamic – eye closure and oral competence. In patients presenting early, this can be achieved by nerve repair or nerve grafting. But, in patients presenting late, more complex reconstructions are required. Managing such patients involves reconstructive surgeries to restore eye closure and facial symmetry, static and smiling. Here we discuss a case that presented late and required such complex procedures.
Case Study
A 33-year-old female patient presented at Medanta-Gurugram with chief complaints including saliva drooling from the right side of the mouth, food pooling to the right side of the mouth while chewing, inability to close the right eye and asymmetric smile due to absence of movement on the right side of the face. The patient was diagnosed with right-sided facial nerve palsy. The symptoms had developed after the patient underwent a surgery to remove brain tumour (vestibular schwannoma at the right cerebellopontine angle). Due to facial asymmetry, she had started isolating herself and sought help to improve her condition. At the time of presentation, the patient was also undergoing radiotherapy due to which nerve repair or grafting was not possible.
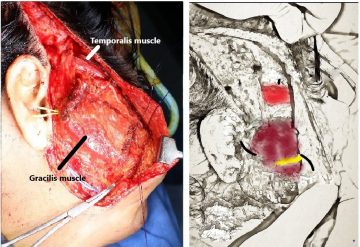
After the completion of her radiotherapy, when the patient again presented to us, her examination showed that the right side of her face appeared to be sagging in comparison to the left. She was not able to raise her right eyebrow, close her right eye completely, frown or smile due to the lack of muscle tone on the affected side of the face. The patient was counselled for reconstruction surgery and was planned for a temporalis transfer for eye closure along with a functioning free muscle transfer for oral competence and smile in a single-stage procedure. Nerve repair or grafting was not an option in her case due to time gap since injury.
In temporalis transfer, a slip of the temporalis muscle was taken along with an extension from its overlying fascia and was routed towards the eyelid. The fascial extension was divided into two strips and one each was given to the two eyelids of the right eye. With the contraction of the temporalis muscle, the eyelids would close to cover the eye.
For the smile and to support the lower lip to prevent drooling, a segment of the gracilis muscle was harvested from the opposite thigh along with its vascular pedicle and nerve. This was brought onto the right side of the face and fixed to the zygomatic bone and to the modiolus (the junction of the
Issue 58January 2023
Dr. Arvinder Singh Soin
ChairmanInstitute of Liver Transplantation and Regenerative Medicine 
Medanta – Gurugram
Dr. Amit Nath Rastogi
Director Institute of Liver Transplantation and Regenerative Medicine
Medanta – Gurugram
Dr. Vivek Gupta
Senior Consultant Liver Transplant & Hepatobiliary Surgery Institute of Liver Transplantation and Regenerative Medicine
and Regenerative Medicine
Medanta – Lucknow
In Focus
muscles of the upper lip, lower lip and other mimetic muscles). The arterial supply and venous drainage were restored using microsurgical anastomosis to recipient vessels in the face. The nerve to gracilis was given two inputs – one from the ipsilateral nerve to masseter (for early reinnervation and to give strength to the contraction), and another from the opposite normal side buccal branch of facial nerve with the use of a nerve graft (for spontaneity of the smile). The use of the slip of temporalis, the gracilis muscle and the sural nerve graft do not cause any significant donor site morbidity.
All these steps were done simultaneously and successfully in a single-stage operation.
The surgery and the hospital stay were uneventful and she was discharged on Day 5 post surgery. The stitches were removed on Day 10 and retraining exercises for the eyes and the mouth were started after 4 weeks. The patient required some readjustment of the muscle attachment to the lips in the follow-up period.


Seven months following the surgery, the patient is doing well. The patient can now close her eyes completely; there is no drooling of saliva, no pooling of food and she has a symmetric smile. The hollowness of the face on the right side is also gone. To conclude, there are options for improving the lives of patients with facial nerve palsy even if they present late. These patients need not live with the functional loss and social stigma associated with this condition and they can be rehabilitated fully.
Dr. Aditya Aggarwal

Vice ChairmanPlastic, Aesthetic and Reconstructive Surgery
Medanta - Gurugram
Medanta Mediclinic Now Also at Subhash Chowk, Gurugram
Taking another step towards making our world-class healthcare more accessible for the residents of Gurugram, Medanta has launched a Mediclinic at Subhash Chowk in Sector 38, Gurugram.
The changing needs of our patients make it important for us to deliver services in a way that they find more convenient. Towards this, and to cater to working professionals, the Mediclinic will remain open Monday to Saturday between 9AM and 9PM. Our superspecialist doctors from over 25 specialties, including heads of departments, will be available for consultation at this clinic.

Services
• Superspeciality consultations by Medanta doctors
• Executive health check-ups
• Physiotherapy and rehabilitation
• Child and adult vaccination
• Dental services
• Diagnostic tests, including lab tests and radiology services as well as specialised diagnostics (TMT,
ECHO, ECG, ultrasound, blood tests, X-ray, audiometry, uroflowmetry)
• Day-care services, such as antibiotic therapy, administering IV medication, suture removal, wound
dressing
• Diet and nutrition counselling

Specialties
Cardiology | Internal Medicine | Gastroentrology | GI Surgery | Hepatobiliary Sciences | Paediatrics |
Paediatric Gastroenterology | Endocrinology and Diabetes | Musculo-Skeletal Disorders and
Orthopaedics | Respiratory and Sleep Medicine | Neurology | Mental Health | Breast Services |
Gynaecology and Gynaeoncology | Peripheral Vascular and Endovascular Surgery | Diet and
Nutrition | Nephrology | Urology | ENT | Dental Sciences | Dermatology
Kudos

Congratulations to Dr. Manish Jain (Director - Nephrology, Kidney and
Urology Institute, Medanta, Gurugram) for being adjudged as the
Nephrologist of the Year at the Economic Times Healthcare Awards 2022.
Dr. Jain has over 20 years of experience and specialises in Renal
Transplantation, Renal Replacement Therapy, Dialysis, and other Kidney
Disease treatments.
Dr. Jay Singh Arora
Consultant – Nephrology
Medanta – Indore
Welcome on board
 Dr. Randeep Guleria
Dr. Randeep Guleria
Chairman - Institute of Internal Medicine, Respiratory & Sleep MedicineDirector - Medical Education
Medanta - Gurugram
Nephrologist with expertise in kidney transplantation, preventive and interventional nephrology, renal
replacement therapy, critical care nephrology and paediatric nephrology.
Pioneer in pulmonary medicine, sleep and metabolic disorders with over three decades of experience
and expertise in interstitial lung diseases, asthma, tuberculosis, interventional pulmonology, COPD,
sarcoidosis, sleep disorders, lung cancer and infectious diseases.
 Dr. Abhinav Chhabra
Dr. Abhinav Chhabra
Consultant – Interventional Cardiology
Medanta – Gurugram
Interventional cardiologist with expertise in all diagnostic and therapeutic cardiac procedures. He
specialises in cerebral and carotid artery stenting in stroke patients.
 Dr. Vivek Gupta
Dr. Vivek Gupta
Senior Consultant – Liver Transplant & Hepatobiliary Surgery
Medanta – Lucknow
 Dr. Mayur Mayank
Dr. Mayur Mayank
Consultant – Radiation Oncology
Medanta – Gurugram
Liver surgeon with expertise in treating liver cirrhosis, hepatitis, liver and biliary diseases in addition to
cancers of liver, gall bladder and pancreas. He specialises in liver transplantation, hepatobiliary and
abdominal surgeries.
Radiation oncologist with expertise in all techniques of radiation therapy, their planning, evaluation
and execution.
Medanta - Gurugram
Sector - 38, Gurugram, Haryana | Tel: 0124 4141 414 | info@medanta.org
Medanta - LucknowSector - A, Pocket - 1, Sushant Golf City,Amar Shaheed Path, Lucknow I Tel: 0522 4505 050
Medanta - PatnaJay Prabha Medanta Super-Specialty Hospital, Kankarbagh Main Road, Kankarbagh Colony,
PatnaTel: 0612 350 5050
Medanta - RanchiP.O. Irba, P.S. Ormanjhi, Ranchi | Tel: 1800 891 3100
Medanta - IndorePlot No. 8, PU4, Scheme No. 54, Vijaynagar Square,AB Road, Indore I Tel: 0731 4747 000
Mediclinic - DelhiE - 18, Defence Colony, New DelhiTel: 011 4411 4411
Mediclinic Cybercity - GurugramUG 15/16, DLF Building 10 C, , DLF Cyber City,Phase II, Gurugram I Tel: 0124
4141 472
Medanta - Mediclinic Subhash ChowkPlot No. 743P, Sector - 38, Subhash Chowk, GurugramTel: 0124 4834 547

