Knowledge Byte: Reverse Shoulder Replacement Procedure
Osteo-arthritis of the shoulder joint is a progressive disorder characterized by damage to the articular cartilage of humeral head and/or glenoid. It can lead to debilitating functional limitations, compromising the individual’s quality of life. Shoulder Replacement is the only solution for such patients.
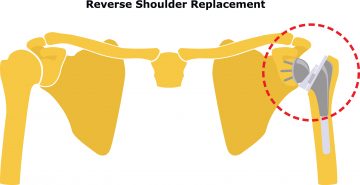
Reverse Shoulder Replacement has emerged as the preferred technique for dealing with longstanding cases of arthritis/ tendon damage/ fractures or complications arising out of previous treatments or neglect. Reverse shoulder arthroplasty has better outcomes than conventional anatomical total shoulder replacement in these complex situations. More sophisticated implants, designs, techniques, coupled with better understanding of the shoulder biomechanics has contributed to the popularity of the procedure. Reverse Shoulder Replacement is designed in such a way that it does not need the stabilizing effect of rotator cuff tendons which is essential for anatomical shoulder replacement to function.
Reverse Shoulder Arthroplasty has proven to be the procedure of choice in the following conditions:
• Arthritis (osteoarthritis, rheumatoid arthritis, cuff tear arthropathy, post-traumatic)
• Irreparable rotator cuff tears
• Comminuted fractures in the elderly
• Trauma sequalae (mal-unions, non-unions,
fracture-dislocations of proximal humerus)
• Failure of previous fixation
• Failure of previous arthroplasty
• Tumors
The Medanta Institute of Musculoskeletal Disorders and Orthopedics has a dedicated Shoulder and Upper Limb Unit which provides world-class care in arthroscopy, joint replacements and fractures of the upper limb. The team has an experience of over 3,500 shoulder surgeries and over 200 shoulder and elbow replacement surgeries.
Case Study
A 65-year-old male reported to Medanta with two-year history of right side shoulder pain which had progressed over time and increased in intensity. He had difficulty moving his right shoulder and performing activities of daily living. He had been misdiagnosed as frozen shoulder and managed with analgesics and intra articular steroid injections elsewhere. The patient was experiencing pain even at rest. Loading of the joint was also painful. He was a known hypertensive and had undergone knee replacement in the past.
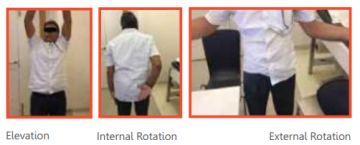
The patient presented with the findings of restricted range of motion with internal rotation contracture of 30 degrees which was limiting him from even accessing his back pocket. External rotation was not possible due to internal rotation contracture, abduction was 70 degrees, and forward flexion was 100 degrees. The strength of muscles could not be tested as loading the arm was extremely painful.

X-rays revealed primary osteoarthritis of the shoulder with Walch B2 biconcave glenoid, erosion of the posterior glenoid with head of the humerus locked posteriorly. In this case, a conventional anatomical replacement would have failed because of deficiency in the socket (glenoid) of the shoulder.
True AP view of shoulder showing Axillary view of the shoulder showing posteriorly locked
glenohumeral arthritis humeral head (Biconcave glenoid)
CT scan was done to measure the exact bone loss on axial cuts, and get an estimate of wedge bone graft required to compensate for the glenoid defect to correct the native glenoid version.