
Emerging Infectious Diseases: A Global Pandemic
Humans and animals have long shared codependent relationships. Both species have historically worked in close proximity to fulfil their mutual needs for energy, security and companionship. However, this close physical proximity has also resulted in the growth and transmission of new breeds of diseases.
Known as zoonotic pathogens, these bacteria, virus, or parasites can move from animals to humans through contact. Although it isn’t clear which diseases moved from animals to humans, there is growing evidence from medical research that epidemic diseases like measles, smallpox, and influenza were transmitted to humans from animals.
“When you bring animals together in these unnatural situations, you have the risk of human diseases emerging,” says Kevin Olival, a disease ecologist and conservationist at the EcoHealth Alliance.
A significant rise in zoonotic diseases, like the recent Wuhan Virus, has claimed the lives of hundreds while infecting thousands of others around the globe. It is important we take note of the emerging infectious diseases and work towards finding cures for them.
What Are Zoonotic Viruses and Why Are They So Dangerous?

Not too long ago, if you were sick or had an infection, your general physician would suggest a drug to cure or treat your illness. It was that simple.
From Penicillin to Paracetamol, antibiotics have been a powerful tool in controlling, treating, and preventing infectious diseases.
However, the rampant overuse of antibiotics has resulted in a new breed of ‘antibiotic-resistant pathogens’. These superbugs are increasingly unkillable by traditional drugs and are evolving to survive beyond their natural lifespans.
Antibiotic-resistant, zoonotic pathogens have already demonstrated their capabilities of causing widespread illnesses in a short span of time with multiple outbreaks such as Ebola, Nipah, SARS, MERS, and Wuhan Virus, that have claimed the lives of thousands over the last decade.
Despite being identified centuries ago, their reemergence has affected public health gravely due to overuse of effective vaccinations and therapies, rendering even the simplest of infections like Influenza a potentially dangerous threat for humans.
It is important to note that the source of these diseases could be anything ranging from bacteria, fungi, to viruses. However, in recent emerging zoonotic viruses, the bat has been identified as a natural reservoir for pathogens.
Some of the most recent viruses of bat-origin are:
Coronavirus
Coronavirus is a cluster of viruses that originates from wild animals and can be transmitted to humans. It gets its name from the crown-shape that is visible under a microscope. In humans, any strain of the Coronavirus can cause respiratory illnesses that can be fatal if untreated. Here are some of the most dangerous variants of Coronavirus:
- SARS: Severe Acute Respiratory Syndrome or SARS is one of the most prominent examples of a zoonotic virus-led outbreak. Believed to have been transmitted by bats SARS killed more than 800 people and infected over 8000 worldwide between 2002 to 2003.
- MERS: The Middle East Respiratory Syndrome, or MERS, is another strain of the Coronavirus that caused havoc in the Middle East in 2012. Like SARS, the MERS also originated in bats and then moved on to animals like the camel. Since 2012, MERS has caused 2,494 confirmed cases in 27 countries and killed 858 people.
- Wuhan Virus: The recent outbreak of a novel strain of Coronavirus, named the nCoV-2019 or Novel Coronavirus, is similar to SARS, and is the newest epidemic plaguing not only China but the rest of the world as well. It originated from a live animal and seafood market in Wuhan City, China, and has been traced back to bats, yet again. Learn more about the Novel Coronavirus here.
Paramyxovirus
Paramyxovirus is a class of viruses that cause respiratory illnesses and diseases like measles and mumps. The Nipah virus (NiV) is an emerging zoonotic virus from the family Paramyxoviridae, genus Henipavirus. It gets its name from Sungai Nipah, a village in Malaysia where it was first discovered. Read more about the last outbreak of Nipah virus here.
Filovirus

The filovirus is believed to be transmitted through ‘bushmeat’ activities – like capture or slaughter of wild animals. However, it can be traced back to the fruit bat species from Gabon and the Democratic Republic of Congo. The last deadly outbreak of a strain of Filovirus was Ebola. Learn more about Ebola and its effects on public health here.
Why Are These Pathogens a Future Global Threat?
While the growth of these ‘superbugs’ is primarily attributed to causes like natural evolution, secondary reasons like excessive antibiotic use have made the situation even trickier.
A study by Clemson University professor, Vincent Richards, states that zoonotic viruses are highly capable of adapting their DNA to survive changes in their environment and hosts.
Furthermore, they have a wide range of hosts, from domesticated animals to human beings, and can be transmitted via simple exchange of food, water, or physical contact, thereby making it extremely easy for them to proliferate.
We can already see evidence of these zoonotic viruses enabling dormant or novel infectious diseases to make their way into animal and human population steadily.
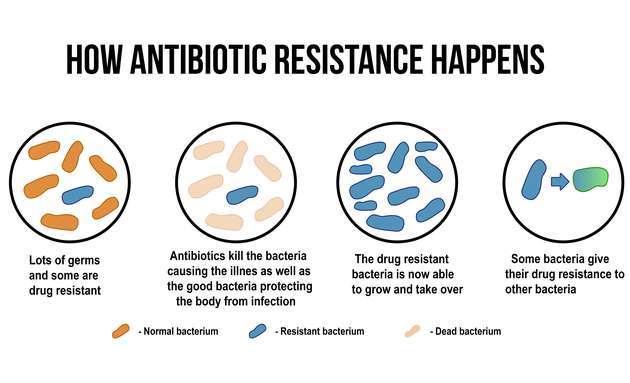
These germs multiply quickly, allowing them to overpower the host’s immune system, resulting in an infection. However, with repeated use of antibiotics in the body, the germs undergo mutations in their DNA and continue to multiply rapidly. While most of the pathogens can be eliminated by antibiotics, there are some that become resistant and dominant. These pathogens then multiply and pass on their antibiotic-resistant genes.
To treat this, a second dose of a different antibiotic may be used. However, if your infection does not respond to the treatment, you may be prescribed another.
This cycle continues and the germ’s adaptability keeps improving, surviving different antibiotic treatments, to finally become a superbug.
The superbugs can spread infections like wildfire, and be resistant to most treatments, making them a huge concern of public health.
So, what can we do to curb the spread of such infectious diseases?

It is imperative that governments, health workers and scientists at every level and in every nation work together to further nurture and minimize such outbreaks.
Although antibiotic resistance cannot be stopped completely, there can be ways in which it can be slowed down.
- Use antibiotics only when necessary
- Take the shortest possible course of treatment
- Don’t use/recommend antibiotics for viral infections
Medical experts are working on developing stronger, more effective antibiotics for emerging infectious diseases. However, until vaccines are developed, it is important we maintain safety and precautionary measures like:
- Maintaining personal hygiene
- Wearing N-95 protective masks
- Curbing the consumption of wild animals/game meat consumption/trade/slaughter
Also, people can fortify their immunity by consuming an immunity-boosting diet and exercising regularly.

